Patient Support
Patient
Resources
As with many under-diagnosed diseases, getting the care and support you need can be challenging. In order to receive the best care possible, it’s vital that you become your own healthcare advocate. The objective of this section is to help you find the resources and information you will need to support your efforts.
FMD Awareness Products
(can ship internationally)
Help us to spread awareness about Fibromuscular Dysplasia!
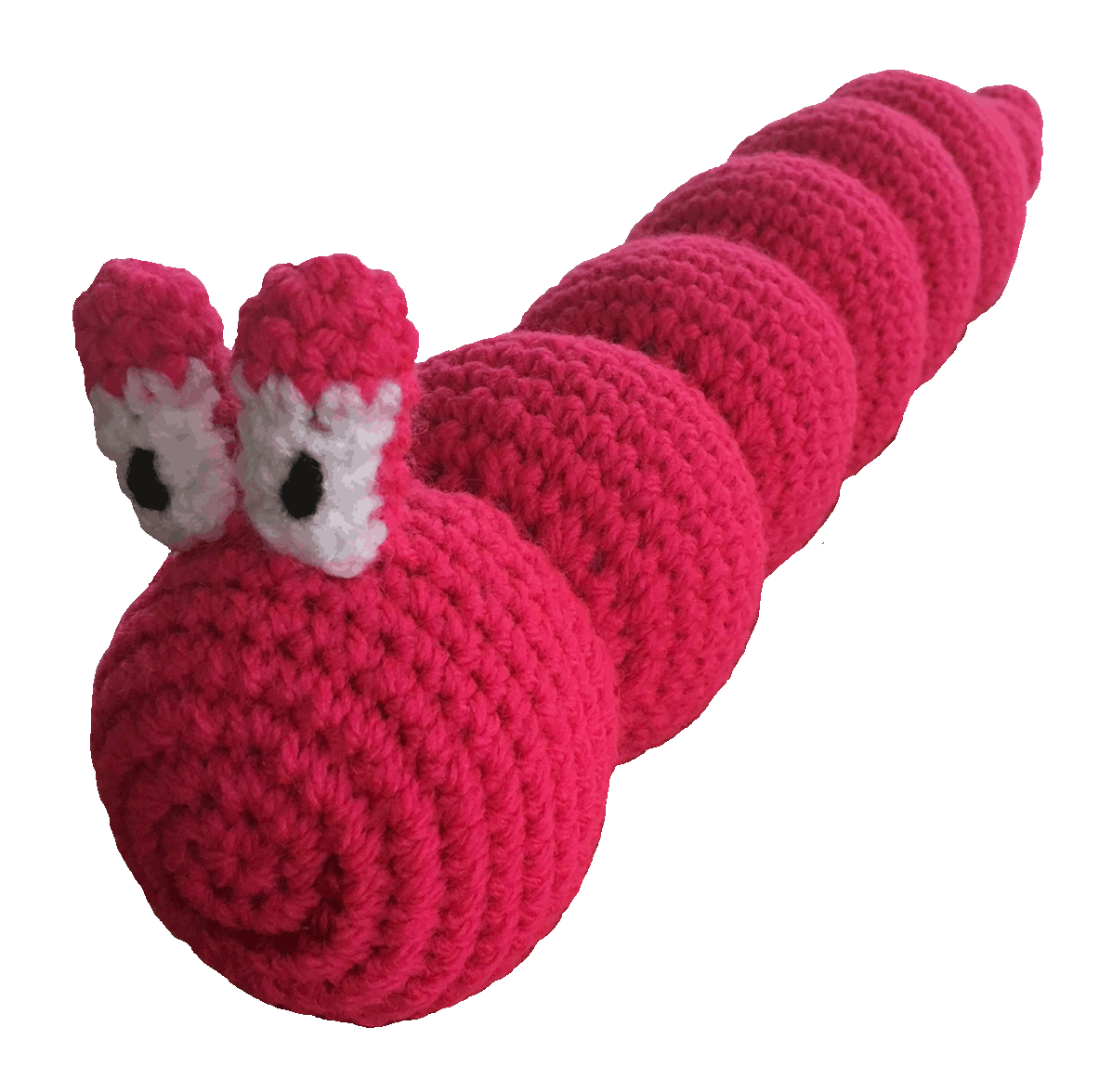
FMD Bracelet Program
 A very special “string of beads” for FMD awareness.
A very special “string of beads” for FMD awareness.
A Letter from our Executive Director, Pam Mace
My name is Pam Mace, and like most of you, I have Fibromuscular Dysplasia (FMD). I was first diagnosed with a left vertebral and bilateral carotid artery dissections after experiencing a TIA (Transient Ischemic Attack or ministroke). I also formed carotid aneurysms that led to several procedures, and a further diagnosis of renal FMD.
With so little information and difficult experiences to deal with, those of us with FMD have evolved into our own little family and depend on each other for support and an understanding of the disease.
In honor of our FMD family, I wanted to create a bracelet that would symbolize the unity among us and raise awareness about FMD. Together with Katie Janoch, jewelry designer, FMDSA has created a bracelet that we feel reflects the diverse challenges we face with FMD and the brilliant glimmer of hope for all of us with this disease.
Beads were chosen in the design of this bracelet to represent the “string of bead” appearance of affected arteries that is classic for the most common form of FMD. Brilliant blue to signify the vascular system and a tree charm to represent both the branches of your arteries affected and life itself. The bracelet is exclusive to FMDSA and will serve to raise awareness about this disease. We proudly offer this item as a symbol of FMD awareness. I hope you join me in purchasing and wearing this very special “string of beads” to unite all of us who support FMD awareness.
Please check back later, as we are in the process of locating a new supplier.
To order your bracelet, please contact FMDSA at admin@fmdsa.org
Click here to print your FMD Bracelet Card to go with your FMD Bracelet now!

Order of The Red Boa
As you can see in the photo above many of our members are wearing their red boas while at the same time supporting Rare Disease day. The Order of The Red Boa was created by member Susan Bell for women diagnosed with FMD. To learn more about the Order of The Red Boa.
Click here and you can print a certificate to remind you that you are not alone. After that, all you need to do is purchase your boa.
General Resources
FMD Dictionary
Resource Links
Online Medical Information - Research
Launched in 1996, www.eMedicine.com comprises the largest and most current Clinical Knowledge Base available to physicians and other healthcare professionals.
National Women's Health Resource Center, Inc.
Healthywomen.org is the one-stop shop for women's health information on the web. This site includes frequently asked questions and consumer tips on fitness, nutrition and disease prevention.
MedlinePlus has extensive information from the National Institutes of Health and other trusted sources on over 650 diseases and conditions. There are also lists of hospitals and physicians, a medical encyclopedia and a medical dictionary, health information in Spanish, extensive information on prescription and nonprescription drugs, health information from the media, and links to thousands of clinical trials.
Health Organizations
Global Genes: Leading rare disease advocacy organization. Their mission is to eliminate the challenges of rare disease. They have developed RARE Toolkits, which we think you may find valuable. Some topics include:

Parenting a Child with a Life-Limiting Illness
Genetic Testing: Is This My Path to a Diagnosis?
Searching for Answers: Contacting Biopharmaceutical Companies Effectively
To view these and other toolkits, please visit their website.
Whooshers.com: Do you experience pulsatile tinnitus or the swooshing noise in your ear? Whooshers.com has a wealth of information and resources. Check out their really cool t-shirts as well.
NORD - National Organization for Rare Disorders, Inc.
A 501(c)3 organization, is a unique federation of voluntary health organizations dedicated to helping people with rare "orphan" diseases and assisting the organizations that serve them. NORD is committed to the identification, treatment, and cure of rare disorders through programs of education, advocacy, research, and service.
Provides education, services, and community-based activities in prevention, treatment, rehabilitation and recovery. Their site provides some very informative patient information on stroke.
A division of the American Heart Association and offers a wide array of programs, products and services, from patient education materials to scientific statements.
Major voluntary health organization, seeks to prevent kidney and urinary tract diseases, improve the health and well-being of individuals and families affected by these diseases, and increase the availability of all organs for transplantation.
American Association of Kidney Patients
Exists to serve the needs, interests and welfare of all kidney patients and their families. Its mission is to improve the lives of fellow kidney patients and their families by helping them to deal with the physical, emotional and social impact of kidney disease.
Non-profit charitable organization created by a group of pilots to arrange free air transportation for any legitimate, charitable, medically related need. This service is available to individuals and health care organizations.
National Stroke Foundation (Australia)
Not-for-profit organization that works with the public, government, health professionals, patients, careers and stroke survivors to reduce the impact of stroke on the Australian community.
Government Resources
Americans with Disabilities Act https://www.ada.gov/ada_intro.htm
The official US government site for people who have Medicare benefits.
The Office of Rare Diseases (ORD) was established in 1993 within the Office of the Director of the National Institutes of Health (NIH). On November 6, 2002, the President established the Office in statute (Public Law 107-280, the Rare Diseases Act of 2002). A rare disease (also called an orphan disease) is a disease or condition affecting fewer than 200,000 persons in the United States. An estimated 25 million people in the United States have a rare disease.
National Institute of Diabetes and Digestive and Kidney Diseases
Part of the National Institutes of Health. This is the Institute responsible for research of kidney disease.
The FDA is responsible for protecting the public health by assuring the safety, efficacy, and security of human and veterinary drugs, biological products, medical devices, our nation’s food supply, cosmetics, and products that emit radiation. The FDA is also responsible for advancing the public health by helping to speed innovations that make medicines and foods more effective, safer, and more affordable; and helping the public get the accurate, science-based information they need to use medicines and foods to improve their health.
The National Library of Medicine is a resource provided by the National Institutes of Health and is considered the most comprehensive library of medical information.
Social Security Administration
Official link to the Social Security Administration.
Health Insurance
The official US government site for people who have Medicare benefits.
Social Security Administration
Official link to the Social Security Administration.
Source for affordable health insurance quotes from a variety of health insurance providers.
Miscellaneous Links
Help with the cost of medications. Also see RxAssist for information about individual US State Drug Assistance Programs.
Patient Toolbox
FMDSA Draw My Life.
(FMD Explained)

Just for fun!
Play our word search puzzle
Beadie Fun Fact
Regardless of initial site(s) of vascular bed involvement, patients with FMD should undergo at least one assessment for intracranial aneurysm with brain CTA or MRA
Download documents
- FMD/Dissection Support Group Webinar with Dr. Heather Gornik - 10/19/2021
- Renal FMD Webinar with Dr. Heather Gornik - 10/18/2022
- FMD and SCAD Webinar Slides - 10/17/2023
- Women’s Health and Menopause with Jean Mariño - 7/19/2023
- FMD and Dissection Support Group with Dr Gornik and Dr Hu - Cerebral Aneurysms - 4/18/2023
- FMD Brochure
- Emergency Card
- Medication Card
- Arterial Map (artery location in the body)
- Dictionary (commonly-used terms)
- Letter to Family and Friends of FMD Patients
- 10 Tips Doctors Should Know About Fibromuscular Dysplasia (FMD) - 2018
- What To Do in the First 5 Minutes of Calling 911 - - 05/14/2016
- FMD and Headache with Dr. Heather Gornik - 1/18/2022
"Faces of FMD" Patient Stories
We’ve started to collect stories from around the world and wanted to provide an outlet for the sharing of these personal experiences. If you are interested in including your story, please Contact Us.
Adult FMD
Dr. DeDe Wohlfarth
DeDe is a clinical psychologist who dissected her her superior mesenteric artery and went on to get diagnosed with FMD.
Continue Reading →
Dr. DeDe Wohlfarth
My name is Dr. DeDe Wohlfarth and I am a clinical psychologist who specializes in children and families who have endured trauma and abuse. I teach at historic Spalding University in Louisville, Kentucky. I love my work, but I also love my family. I live with my husband and our four teenage children, who, despite being teenagers, are still wonderful people. ¾ of them currently have their driver’s permit, so every day helps me practice patience. We live in a 1918 farmhouse in rural Southern Indiana that we are constantly remodeling. I try daily to connect with God through prayer and meditation. I am an avid athlete who enjoys running, weightlifting, and yoga. I am also an Fibro Muscular Dysplasia (FMD) patient.
My FMD story goes like this: About five years ago, I was swimming at our local YMCA when I had a terrible pain in my chest, like being stabbed. After trying to ignore the pain for a few days (dumb idea), I eventually went to my doctor and immediately was admitted to the hospital. I learned I had a 5 cm. tear in my Superior Mesenteric Artery, the main artery that runs from your heart to your stomach. The next few months consisted of pain, misdiagnoses, painful tests that I couldn’t afford, and gloomy prognosis. Every medical professional I met differed on what was wrong, but all reiterated that I should have died and was lucky to be alive.
Fast forward through 6 months, when I finally get diagnosed with multi-focal FMD and find the incredibly competent and loving Dr. Gornik and the entire amazing staff of the Cleveland Clinic. Here are some of my learnings from the journey:
- Become your own health advocate. Read research articles. Ask questions, even if your doctor gets annoyed. Trust that you know your body better than anyone else.
- Almost dying/ living with a chronic disease gives us clear perspective on what is really important in life and how we want to live your days. If I could take away my disease magically, but lose the spiritual growth that came with it, I would choose to keep them both.
- Some friends are willing to walk in the cave of darkness with you. Other friends just wait on the outside of the cave in the sun, and say things like, “Let me know if you need anything.” Those friends who show the courage to face the darkness with you are true treasures.
- Embrace today. Yes, we live with risks of future dissections, aneurysms, and strokes, but I am alive to write this. You are alive to read this. Every day brings something good; find it and celebrate it.
- You can still have an active and rich life with FMD. No, I can’t skydive and ride rollercoasters any more, but I still do obstacle course runs, go kayaking, and this summer, I hiked Angel’s Landing at Zion National Park.
- Let’s work together to truly build health care that works: Where doctors listen to patients; where mental, physical, and spiritual health are seamlessly integrated; and where all people, including people of color, poor people, and LGBTQ+ people, have equal access to high quality health services
Abbie Levy
Shares her story of aneurysms, stroke and getting the diagnosis of Fibromuscular Dysplasia.
Continue Reading →
Abbie Levy
While putting on my makeup getting ready to go out to dinner I noticed my right eye was dropping. The following day I saw my Internist who sent me to my Neurologist. We spent most of the appointment talking about my migraines which seemed to be increasing. He had suggested I have an MRA because of the drooping right eye, but the conversation had gone elsewhere and I was about ready to walk out the door when he said, “Why don’t you have that MRA”. The following morning I had the MRA and nothing could have prepared me for the call from my Neurologist a couple of hours later. I was told they did think I had an aneurysm and needed to have a CTA the following day. My parents had just moved to a Retirement Home in Atlanta, my daughter was scheduled to deliver my second grand son two weeks later and I was starting a new Interior Design business. Life could not have been better.
The CTA confirmed the aneurysm and I was sent to a Neurosurgeon for further evaluation. That resulted in a Cerebral Angiogram. The recommendation was to do nothing about the Aneurysm. In fact they actually found two, but they were small and highly unlikely to rupture. As so many of us with FMD often say, “I felt like a walking time bomb.” What I didn’t know that day was that they found much more.
Six months later while reading a book in bed stroke symptoms began. The right side of my face suddenly went numb, I got up and realized I had a very hard time walking to the bathroom. I tried to google “stroke symptoms” and my right hand was uncoordinated and I had a hard time doing it. Living alone I had not spoken all night so didn’t know until I called my daughter that my speech was very slurred. Once I heard myself talk I made the call to 911. I was very puzzled since I didn’t have any risk factors for stroke. After being diagnosed with a TIA and spending the night in the hospital I decided I needed to get that Angiogram report. I got quite a shock when I saw that I had some disease called Fibromuscular Dysplasia in both Carotid and Vertebral Arteries and also in my Petrous, Cavernous and Supraclinoid segments of my Internal Carotid Arteries.
Then there was more.....
The CT scan they did after the Angiogram showed that I had encephalopathy in my left frontal lobe from previous ischemia.
Katie Long
Hi everyone! My name is Katie Long. I’m a 37 year mother of two awesome teenagers in South Carolina. I was diagnosed with FMD in 2012 after a series of strokes. The last thing I ever saw clearly was my friends daughter’s laughing face at her three year old birthday party. Her birthday happens to be perfectly poised to fall on Labor Day weekend, and her birthday parties are a blast for adults and kids alike. We had been swinging into a huge foam pit, and we were having so much fun that the party ended up running two hours over. To this day I still wonder if the swinging led to what followed, but the doctors never really had an answer. After the last swing in I was helping my friends’ daughter out of the foam pit when the aura and headache slammed into me at the same time. I very gingerly got out of the pit and called my kids and their friends together; I told my friend and my sister that I had a migraine with aura. My friend, being also a life long migraine sufferer, knew right away how I felt. I didn't know how to put into words how different I was feeling, how the world didn't feel right and nothing made sense. Or how my mouth had already gone numb on one side and i couldn't feel the left side of my chest.
We packed up the cars as fast as we could. By that point my nausea was nearly overwhelming. Somehow, I got my children’s friends safely to their homes and at our house I remember emptying the dishwasher. My daughter asked me for help with her math homework but I couldn't make sense of anything. My sister told me to go lay down, that she would help her, and I stumbled to my room in a painful haze. My fiancé came by and was concerned enough that he felt I should go to Urgent Care. Now I had had migraines with aura my entire life, but I had never needed to go to the doctor for one.
By the time we got to Urgent Care the numbness had spread from the left side of my face, down my chest, to my left hand. It actually hurt to think. The doctor diagnosed me with a super migraine, gave me a shot of pain medicine and told me to stay home from work the next day. The shot took enough of an edge off of the pain for me to eat a few bites and then pass out in a strange haze at home. My daughter was 10 at the time and very much in the habit of sleeping with me. That night she woke up because I was mumbling and shaking, she called my fiancé and told him I couldn't talk right, that my words weren't making sense, and something was seriously wrong. He came right over and took me to the emergency room. Where we sat for nearly four hours before being seen. By then the numbness was at my hip and they wheeled me back in a wheelchair. A CT scan was ordered, and I was told, again, that I was just having a super migraine. More drugs, and three days off of work this time. I spent that entire day in a haze. I remember my TV was on Nickelodeon and Spongebob played all day. I didn't have the energy or mind frame to turn it. Thankfully, I have an awesome sister, she took care of my kids and me, and I was just waiting and hoping the pain would pass.
That night when I got up to use the bathroom my leg had gone numb. I remember looking down the hallway towards my sisters room thinking it was a million miles away. Leaning against the wall I dragged myself down there and threw myself through her door. She quickly called my parents. They were there in five minutes and my dad took me back to the emergency room. Where we sat again for three hours. This time though they ordered an MRI. I remember the guy saying it would only take twenty minutes. I drifted while I listened to the music they played. Then the guy came back and said it would be another twenty minutes. And that was when I passed out. Hours later I woke up in a hospital bed covered in monitors, IV in each arm, and my parents staring at me with tears in their eyes. The doctor came in and that was when they told me what had happened. I had had four strokes, the initial headache was the beginning, and first stroke, also the one that had damaged my eyesight. I was 34 years old and I had had four strokes. Two in my left lobe, one my right and one in the thalamus. Even the nurses kept saying I was the youngest person on the floor. Yay:/.
At that point they had absolutely no idea why I had had the strokes. I was in the hospital eight days and finally they ordered an Arteriogram. Generally done sedated I had to be fully aware
because of the strokes. The nurses argued with each other the whole time. I was laying on this table with a doctor sticking a line through my femoral artery and these two can’t get it together.
The neurologist came in to diagnose me with this crazy disease no one had heard of Fibromuscular Dysplasia. What. Ok, so what now? Shockingly, I was able to fully recover physically, with the exception of the tips of my fingers. But my scrambled brain couldn't unscramble my eyesight. I tell people it’s like watching TV on a bad channel all the time. If you have migraines with aura then you can understand, that’s how I see permanently. Sometimes when I look at a sidewalk my brain wants there to be people there so I see ghost imagines my mind has “created.” In rehab they told me it’s the brain trying to compensate.
At my job I was the boss and the human resources decided that my medical condition wouldn't allow me to do the job anymore so I wasn't asked back after my six month medical leave. That was a blow because of how much I had put into the company, but with my eyesight being what it is I do understand. But a former boss offered me a new job so I went back to work. Even though migraines went from a passing nuisance to a weekly problem, and I had to take Plavix daily and learn how to deal with seeing the world differently, I was feeling like I was becoming me again. Fast Forward a year and a half. I was headed to work one day when I suddenly got a mind numbing head ache, overwhelming nausea, and my hand went numb:(. I happened to be right next to an Urgent Care off the interstate so I went there, because there was no way I was going to make it to the hospital. I stumbled to the counter and told the lady it was an emergency, I had a history of stroke and had all the symptoms of another one. And she told me, “Stroke or not you have to wait you turn.” I broke down, hysterically I called my sister and she told me to call 911. So I did, they were confused why I was calling from Urgent Care, but by the time I got to the hospital I was convinced I was wrong. I had just started a new medicine and thought that I was having a bad reaction.
Unfortunately I was wrong. The doctor said he was sorry, he could see the other four strokes, but this one was still developing. This one landed me in a rehab facility. By the next day I had
problems swallowing, and even now without spellcheck writing can be a serious issue. This stroke hit on the right side again, and I had to be retrained how to walk. I had to eat my food pureed like baby food, because I couldn't swallow right. I think the weirdest thing was that my hand wouldn't write what I wanted it to write, the connection from my brain to my hand was screwed up. Anyway, I loved rehab, except being watched taking showers, seriously, I no longer have any shame , lol. The therapists and doctors were all so wonderful and kind, and helped me tremendously, even with deficits from my first strokes.
When I have headaches now I sometimes go numb. I have to go to the hospital every three months or so because i ‘ll get one so bad we just aren't sure and all of my doctors say I need to go at the first sign of a stroke. I have started seeing a specialist now for FMD. I have bilateral Vertebral FMD. All my doctors say the same thing, they don't understand why I have had five strokes. They are definitely from the FMD, but five is excessive. With each one my vision gets worse too. Three of the five have happened in my in my occipital lobe. I went from being a perfectly healthy person with a great job and high energy, I loved to jog and go on adventures with my kids. To taking thirteen different pills a day to stay afloat.
After my last job didn't extend my FMLA, I applied for disability. Its a lie that everyone is turned down the first time. I was approved fast. That made me sad, actually, I didn’t need an attorney or
anything. I was just sick enough. I just turned 37. I have no intention of this being my forever. I still think that I can get my health under control and get back out there. There is way too much life left in me to wait around to die. The bad part about having a disease nobody knows or understands is that people look at you and think that you look ok, you must be exaggerating.But on the inside FMD makes you feel like a Jackson Pollock painting.
I think its weird when the doctor tells me my blood needs to be as thin as possible. I think its sad when I wake up and just want to go back to sleep. I hate that I move in slow motion because I
don’t have the energy for anything else. But the absolute worst part about all of this is on my good days, when I forget for a while and live my life normally, because for a moment I feel ok, I
end up paying for it with a monster of a migraine. Or I sleep for two days. Or i end up in the hospital.
Deb Kauble
I have been on medication for high blood pressure since I was 13 years old. Over the years my doctor would tweak my meds
Continue Reading →
Deb Kauble
Over the years my Dr would tweak my meds once in a while but generally it was fairly well controlled. Then in 2012, I fainted. I had never fainted in my life. My husband called an ambulance. On the way to ER, my blood pressure was 245/130. Once I arrived they did all kinds of tests on me and administered several different meds, trying to get my blood pressure down. When they had gotten it to about 150/85 they sent me home and told me to call my family Doctor. She got me in the next day and my blood pressure was up again despite my meds. I told her I felt like something was terribly wrong inside me and if we didn't find it I was going to die. She sent me to the hospital for a CT scan of my kidneys and adrenal glands. Within 5 minutes of me arriving home, my phone was ringing. It was my Doctor telling me she thought I had FMD in my right renal artery. She sent me to the Corvasc Group in Indianapolis, who immediately scheduled a test to go up into the artery thru my groin. I was scared silly but it really wasn't bad. I heard the Doctor remark about the amount of webbing he saw and he started ordering balloons. He went ahead and cleared out all the webbing right then. Before the procedure my blood pressure was 180/90. In recovery it was 100/60. They were ecstatic that it had responded so much so quickly. He said that was a good sign and that it was quite possible I had been born with this and this was what was causing this as a child. They did a scan of my abdominal aorta and my carotid arteries before I was released. I go back now once a year to have my renal arteries checked and every 5 for the others. I have since lost 90 pounds and am currently on NO medications for the first time, I am grateful to my family Doctor for listening to me and for the Doctors at Corvasc in Indianapolis for fixing me! I pray it doesn't come back anywhere else. I am a 56 year old female. My older sister has had multiple strokes due to vasculitis in the brain, my Aunt and 2 uncles died from strokes and another uncle died from a ruptured abdominal aorta. I feel blessed to have found this and that we are able to keep a close eye on things that might spare me the same fate.
Sincerely,
Debbie Kauble 2015
Phyllis Baker
Well, here is my story. My name is Phyllis Baker. I was born and raised in New Orleans, LA until we were transferred here in Houston, TX in 2003.
Continue Reading →
Phyllis Baker
Well, here is my story. My name is Phyllis Baker. I was born and raised in New Orleans, LA until we were transferred here in Houston, TX in 2003.
I was a very happy, healthy, 16 year old girl in 1978. I had some migraines, and so my blood pressure was checked and it was always fine. This turned out to be hormonal, and not related. Because of my doctors’ visits and blood pressure checks, this turned out to be an important key in knowing exactly when the FMD showed its symptoms.
Well, one day I was very sick with a bad throat and all the symptoms of Mononucleosis. It was a Sunday and I felt awful, so my Mom took me to a little clinic in the office building of my doctor; Dr. Kirk H. Webster. He was at Methodist Hospital in New Orleans East. It was open on Sundays. He happened to be on duty. I just remember feeling horrible and hoping I didn’t have Mono. There was no
doubt I had it and I knew exactly who gave it to me! LOL
They examined me and my blood pressure was 215/180. Because of the headaches, it was documented before that and it was never high. Well of course they checked it over and over with me standing, sitting, lying down... I remember them telling me to lie down and try to relax and they turned the lights out while I lay on the uncomfortable bed. I was thinking. Gee Wiz, I'm miserable with my throat and all my Mono symptoms. Just give me some medicine and let me go home. They eventually did send me home with medicine for the Mono and instructions to my Mom to come back after the Mono was gone so they could check on my blood pressure. I remember only being concerned with getting over Mono, and missing my exams in high school.
It was May, and so as soon as I could, I made up my exams and my wonderful Dr. Webster started testing me. Right away. He was not going to stop until he found out the reason for the High Blood Pressure. God Bless him! I was first put on a low sodium diet, (that was lovely and impossible in 1978), and medications for the pressure which didn't do much. After several tests, including those fun old IVPs, I was diagnosed with Renal FMD. This was within 2 months. I cannot express to you all how incredibly blessed I feel being diagnosed so quickly back then. I, like many, was told it was extremely rare. Over these past 34 years, and still now, whenever I would go to a doctor, dentist, etc., no one had ever heard of it. When I discovered the FMDSA site, I was blown away reading about so many of you who lived with horrible symptoms and were dismissed or missed diagnosed!
Anyway, in 1979, a local surgeon in N.O., LA did a bypass on my left kidney. He used a pig's vein. His intentions were great, but it was uncharted territory and it failed. I had FMD extensively in both kidneys. For years I was tested over and over again with angiograms and anything they could think of to help me and learn more. They did go in one time during an angiogram and were going to attempt a brand new thing. Angioplasty. This was probably in 1981. They didn’t even try once they looked closely while doing the Angiogram. My arteries were too tightly closed. For several more years I was watched and given blood pressure medicine, and of course the low sodium diet. It’s funny, but I was really devastated over the OLIVES! LOL. I know it sounds silly, but when I found out about the sodium in olives and that I could no longer eat them, it was awful. I was 16, but really! (I have to admit, I eat them now in moderation.) Back then of course, there were very little low sodium products. Thank God my mom was a fabulous cook.
Then, life just went on. I went off to college and got married to my wonderful husband of 27 years. During these years in college and my first year of marriage, I was on many blood pressure medications and checked on often. It was getting pretty out of control and so in 1986, my doctor told me of a wonderful Nephrologist, Dr. Figueroa, at Ochsner Clinic. I began seeing him and he treated me for years. He knew of a friend of his at Cleveland Clinic who could possibly help me. He was to do bypasses on my right kidney. They could only do one at a time and by this time; the left kidney was full of scar tissue. So in 1986, I traveled with my sweet mom and husband of 1 year, to CC. The surgery was a great success. The incredibly talented, late Dr. Novick did a nine hour surgery with several tiny bypasses on my right kidney with veins from my leg. It was a complete success and I came home Christmas Day. What an incredible surgeon. I was so saddened to hear he died a few years ago. Such a great loss. After a couple of months after the surgery, the pressure was under control. It has improved dramatically and is monitored. I was then able to even have 2 children with this disease! My blood pressure was and is under control. My left kidney has atrophied so much it actually helped the pressure go down over time, with less pressure on these arteries. My one kidney is doing fine.
So, as I sit in awe, of what seemed to be for me, a lonely disease, I am blown away learning about so many who have suffered and died because of the lack of knowledge of this disease, and or
misdiagnosis.
So that's my story. I have been blessed to live a good life so far. I was able to enjoy my high school and college years and so on. Praising God for this!
I'll share one more thing. I can remember crying at night to my mom, as she took that extremely high blood pressure. No automated cuff and Velcro back then. It had to be tied on my skinny arms! Ha,
things have changed for me in that department. Of course it took so long as she pumped that pressure cuff up past the 250 number and slowly listened with a stethoscope. I remember crying and telling my mom that I wasn't going to live to be 40. She and my Dad always encouraged me and really most of the other times I was able to not even think of it and have a great time. I really had a gloriously happy time most often in those early years. Now, here I am, 49 1/2 years old!
I was so very blessed to have been able to receive the proper care and attention. I have been so blessed in many ways in my life. I have a wonderful husband and family. My parents and siblings
were so loving and caring all those years ago, and I still have my mom with me at 88 years old!
Since I have found FMDSA, I have wondered WHY. Why me? Not the “Why me?” you might think I mean. I mean WHY DID I GET THE PROPER DIAGNOSIS AND HELP WHILE SO MANY OTHERS SUFFER NEEDLESSLY? I was in N.O., a large city with great medical care, but I started out at little local hospital and Internist. I know it was Dr. Webster. He was an amazing and brilliant doctor to me.
He was just not going to give up on me till he found out what the problem was. It is incredible. I was not in the middle of a place like Cleveland Clinic or even here at the wonderful world renowned
Medical Center in Houston, where there would have been a better chance for this to have been caught. But still, why me? Why did I have the gift of Dr. Webster and all that followed? Lately I have
really been thinking about this a lot. I know God has a plan for everyone, but it is still so hard to get. How could I go for so long not knowing others had it either? I do know that over the years I told every doctor, dentist, nurse, and anyone who I came in contact with medically, and no one really ever knew what it was, so I did not look further to see if there were others out there. I can only hope that by finally officially telling my story is the beginning of doing my part in spreading awareness of FMD. I am so thankful to FMDSA, Pam Mace, and all the doctors and volunteers involved. I am looking forward to one day making the conference in Cleveland. I know it will be great to get to know others like me.
Andrea Bettoni
Hi, my name is Andrea Bettoni, in spite of my name I’m a 33 male. At the age of 31 I suffered from a heart attack, during a morning run.
Continue Reading →
Andrea Bettoni
Hi, my name is Andrea Bettoni, in spite of my name I’m a 33 male. At the age of 31 I suffered from a heart attack, during a morning run. Fortunately I was close
to my parents’ I was immediately hospitalized and I was put 2 stent. No doctors thought that it could be suspected to have a heart attack at that young age & with apparently excellent medical conditions (except the fact that I was a smoker!!! ).
Since that I kept continuing have chest pain until I was hospitalized again and put a third stent. My conditions, unfortunately, didn’t changed: being not convicted of the reasons of my heart attack and the misdiagnoses of the doctors I went to ( fortunately my oldest sister I a doc…. ), I underwent a whole series of scans and tests. I’ve been visited by a haematologist that prescribed new blood tests, I found out I suffer from a genetic mutation called MTHFR 1298 – Homozygous. I kept on searching for the disease I was suffering, I wasn’t satisfied & and most important, I wanted “my life” back. Looking back now, I can say that that thought helped me the most. I had a coloured ecodoppler that revealed that I had a lots of very small clothes in every artery; doctors tried to destroy them by giving me aspirin but the clothes grew up until there was 90% occlusion of the superior mesenteric and the internal left carotid: a biopsy has been made on my right temporary artery & “finally” I had the response: I was suffering of Fibromuscolar Dysplasia.
By this time I can say that I’ve been lucky because the carotid stenosis grew until 100% twice: I just suffered from some worst headaches with no other consequences. Nowadays I’m pretty fine, I just have to take my pills everyday and one ecodoppler a month : after all, I still consider myself a lucky one, maybe just because I’m still here & can talk about my “bad experience” hoping that it can be useful for somebody else.
Mimi Petersen
I remember when I was a little girl how interested the doctors were always with my abdomen.
Continue Reading →
Mimi Petersen
I remember when I was a little girl how interested the doctors were always with my abdomen. While doing a routine check8up they were always commenting on my bruits. Being young I was very proud of these, after all I was unique As I became a teen I realized that perhaps these bruits were not necessarily a good thing. Yet there was never any testing just a lot of "hmmmmmmmmm" 's.
By the time I was 16 my blood pressure readings were beginning to be high. Of course being still very young, I assumed if there was a problem it would be addressed. At 18 years old a medical facility outside of my HMO informed me that I had hypertension and should address this with my primary doctor(s). This was when I was "officially" diagnosed with hypertension. No longer being given the 'white coat' diagnosis, hypertension was now acknowledged. Unfortunately I was not given any type of work up to determine the cause of my hypertension (although I had bruits in my abdomen area). I was told to not smoke (which I didn't and still don't), not to take birth control pills (I went off the pill), and to be prepared that I could have a stroke by the time I was 40. I am pleased to say that I am now 51 and have yet to have a stroke. But, with years of hypertension behind me this is a true and great fear I have. It was now the norm for me to hear from every doctor visit "you are to you young to have hypertension". Yet still no arteriograms, or further investigations. I gave birth to my first son at the age of 26.
I had pre8eclampsia during delivery , with a bevy of doctors in the delivery room. I was very scared. I was told after that birth that I should consider not having any more children. Not yet being the assertive and inquisitive woman I am today (and with out the advent of the internet), I was not quite sure of the reasoning behind that statement. So I forged ahead and had baby number two. As I remember my B/P was rising and there was some concern during delivery, but my second son came at rapid speed and the birth was far less eventful than the first. When I was 28 years old, it was finally determined that I needed an arteriogram to check my kidneys. At this point I was told that I had an atrophied right kidney due to birth defect. I was put on B/P meds at this age. Ten years later when I requested medical records there was a notation of Renal Artery Stenosis. The turning point in my medical care came at the age of 39.
My B/P was still high on two meds. If it had not been for a friend who was a nurse and insisted that I pursue this, I might still not have been diagnosed. I left the HMO that I had for 39 years. When I met with my new internist for the first time, he said my B/P was not acceptable for someone my age. He asked me who was my nephrologist. I did not even know what a nephrologist was. I was immediately referred to one. Everything started moving fast from that point. I had rennin samplings done on my 'atrophied' kidney and an arteriogram done on my other renal artery. It was at this point that I was diagnosed with Fibromuscular Dysplasia. My understanding is that the FMD was what had caused my left kidney to atrophy as the renal artery had become severely stenosed. It was emitting a high amount of rennin (a nasty hormone that was increasing my B/P. Also my right renal artery had Fibromuscular Dysplasia.
The suggestion was to embolize (coil around the artery to render it lifeless) the left kidney to stop it from producing the high amounts of rennin. Also I was to have angioplasty on the right renal artery to open it up for better blood flow. By this time I was using the internet and trying to advocate for my health. There was not much available at this time (1999), like there is now, none the less it was very helpful. I also had a second opinion at UCSF before I went ahead with the embolization. They agreed that it was in my best interest to stop that kidney from preventing the rennin. I had both the embolization and angioplasty done in 1999. Unfortunately years of hypertension are not so easy to get under control. I was back in for another angioplasty 4 months later.
Through the years I have had approximately a total of 14 arteriograms/angioplasties. I have been on numerous B/P meds. In 2006 my right renal artery appeared open and clear. Yet my B/P has remained high. A few doctors suggested looking at the embolized kidney to see if it perhaps it was still emitting rennin. It had been noted that there was a collateral artery that was still feeding this kidney and helping it barely hang on. Turned out that kidney was emitting a significant amount of rennin. I had left kidney removed by laparoscopic nephrectomy in March of 2007. The procedure seems to be a success as I have been able to reduce my B/P meds in half.
In addition to my renal FMD, I have carotid and mesenteric involvement. I am being followed by a wonderful Vascular Doctor at UC Davis in Sacramento. I have follow up ultra sounds every six months to monitor the status of my FMD. It is my hope that in sharing my story it will bring awareness to this disease. I feel because of the efforts of the Fibromuscular Dysplasia Society of America , that perhaps other children will not have to suffer a lifetime of hypertension due to lack of diagnosis. Furthermore also having FMD in my carotids, I think it is imperative to share with health care providers that FMD has been recently recognized by the National and American Stroke Associations as a cause of stroke.
Sometimes I am frustrated about all the medical care providers who are not aware of this disease. Yet I take great comfort in knowing that I am spreading the word about this disease. Mimi Petersen Sebastopol, CA imim1256@yahoo.com
UPDATE: Nephrectomy was done 3/2007 There has been a reduction in B/P meds.
Jodi Roth
Hi, my name is Jodi Roth. I am a 38 year old mother of two young daughters and I have fibromuscular dysplasia of the renal arteries.
Continue Reading →
Jodi Roth
Hi, my name is Jodi Roth. I am a 38 year old mother of two young daughters and I have fibromuscular dyplasia of the renal arteries. My journey with this disease began by accident in May 2004 while I was sitting at my kitchen table having a medical exam for a life insurance policy. The doctor took my blood pressure and it was extraordinarily high so I followed up with my internist. My internist was quite surprised how high my blood pressure was given that I am thin, in good physical shape, eat pretty healthy and don't smoke or drink. After several months of doctors visits, medication and many tests, a local Cardiologist heard a brui in my renal arteries and sent me for a renal MRI. When he called me and asked that I come see him, I knew the results were not good. Later that day he told me in person that I had Fibromuscular Dysplasia in both renal arteries and that I had an
aneurysm on my left renal artery.
My life flashed before my eyes, and all I could think of was that I wouldn't see my young daughters grow up. I was devastated. Then, of course I started researching this disease and tried to learn as much as possible about it as I could. I found the FMDSA website which educated me a great deal about this disease and I immediately became a member of FMDSA. I went to an Interventional Radiologist for angioplasty on my right renal artery and an attempt to cut off the aneurysm on the left renal artery, but it was unsuccessful as the aneurysm was too close to my kidney. I was then referred to Dr. Andrew Novick at the Cleveland Clinic and in January 2005 underwent renal bypass surgery on my left renal artery to remove the aneurysm. It was a long and difficult recovery, but luckily it was without major complications and my blood pressure went back down to the normal range. I go for renal scans every 6 months and recently had an angioplasty on my right renal artery which had re-narrowed. Physically I feel great and I continue to exercise 3S4 times a week doing cardiovascular activities and strength training, and I try to live a very healthy lifestyle. I have a wonderful life with my husband and kids and I keep an extremely positive attitude about this disease. It's not going away, but as long as I am vigilant about getting scans and seeing my Vascular Dr., it is very controllable. Like many other FMD patients, I want to know how I got this disease, if my daughters will be affected by this disease and how it may affect me and others throughout the years. That is why I believe it is so important to help raise awareness of this unusual disease and to continue to support the FMDSA.
Lisa Fettig (Pregnancy and FMD)
My name is Lisa Fettig. I was diagnosed with FMD in both renal arteries 3 years ago, when I was 34.
Continue Reading →
Lisa Fettig (Pregnancy and FMD)
My name is Lisa Fettig. I was diagnosed with FMD in both renal arteries 3 years ago, when I was 34. I am a dietitian in a dialysis clinic. We were checking everyone’s blood ressure at work one day and discovered that mine was quite high (180’s/90’s). It had always been normal in the past. I considered myself to be quite healthy (normal weight, exercise regularly, eat well, etc.). I didn’t have any symptoms. One of the ephrologists that I work with said I probably had FMD. I had never heard of it.
She ordered all kinds of tests to rule out other things, which all came back fine. The last thing was to do the renal angiogram, which showed the classic string of beads appearance. Angioplasty was done and my blood pressure came right down to normal. I thought I was cured, but within a week it started going back up and I started medication. Since I was kind of trying to get pregnant, Labetalol was used. I hated it because of the side effects, but it did keep my BP under reasonable control. I suspect that I have carotid FMD, also, but it has never been diagnosed. I had a carotid ultrasound, which was normal, but I have had some of the symptoms (optic migraines, swooshing noise in ears sometimes, etc.) of carotid FMD for the past 20 years.
Last Februrary, I found out I was pregnant (first child). I saw a high risk OB, who told me I had a 50% chance of preeclampsia. I was scared to death of that or a stroke. By March I had to stop the Labetalol due to low blood pressure. My blood pressure stayed in the 110’s – 130’s the entire pregnancy without any meds, which was great. I walked almost everyday and continued lifting weights and riding a bike a couple times a week throughout the pregnancy. I gained 25 pounds or so. My nephrologist did some basic labs and a 24 hour urine early in the pregnancy for a baseline, but then she went out on medical leave and I did not see a nephrologist the rest of the pregnancy. Due to my age and BP history, the OB ordered regular ultrasounds (I had 6 total) to make sure the baby was growing appropriately. I also had to go for nonWstress tests twice weekly during my last trimester. That was a pain, but worth the sense of security.
In October, 10 days early, I delivered a healthy 7 pound baby girl. There were no major complications during the delivery. Within a week of delivery my BP started going back up and I went back on Labetalol, because I was breastfeeding. When I stopped breastfeeding, I was able to switch to an AceWinhibitor, which controls my BP very well with few side effects. The baby is now 5 months old and we’re both doing great
Shannon Shivers
Feb. 16, 2008 was a day that can be recorded as a day of miracles! I was 31 (now 32 since November), training for a half-marathon.
Continue Reading →
Shannon Shivers
Feb. 16, 2008 was a day that can be recorded as a day of miracles!
I was 31 (now 32 since November), training for a half-marathon, and had received top reports from my yearly physical just 2 weeks before. I woke up that Saturday morning and stumbled my way to the bathroom, almost making it there, falling in the doorway I could not pull myself up and didn't understand what was going on. I had to call my 4-year-old son, my hero, and tell him to go get mommy the phone and a pillow and blanket, because I was freezing!
He brought the phone, and I called my husband at work. I didn't call 911 because I didn't know what was going on and didn't want to scare the children. He answered saying how surprised he was I caught him because he hadn't been in the office all morning!
He heard it in my voice. My speech was slurred and he knew immediately that something was terribly wrong. He was on his way and called 911 and his parents on the way home. By warming up, I was able to get up and make it to the den, but that would be it. I was paralyzed completely on my left side. Danny made it home in record time, his parents made it over to pick up the children before the ambulance came, and the ambulance soon followed. I arrived at the hospital with complete awareness of everything that was going on. Long enough to hear the doctor verify that I was having a stroke. I then had a grand mal
seizure.
The Dilantin they administered pretty much spaced me out from then on. The doctors had told Danny that the seizure would prevent me from receiving the medication used to stop the stroke and their was nothing else they could do. Danny just said that wasn't acceptable!
The ER doctor, thankfully, had the number of a neurologist that he thought could help. He was training for a marathon, and they called him in on a Saturday in his running clothes! They confirmed that my right carotid artery had dissected 100% and the doctor's suggestion to Danny for any hope was surgery. He signed the consent and they took me into surgery for 6 1/2 hours to place 2 5mm metal stents in my carotid arteries through my femoral arteries!
Amazing!
I woke up after the surgery with complete feeling on my left side The paralysis had left me and I was going to be ok, with no therapy at all. Still in ICU on day 2 with the catheters still in my arteries, the doctor came in and told me I wasn't going to get any running done like that My family's jaw dropped at the thought of me running after that, but he said I could run when I felt like it and expected to see pictures of the marathon.
I left the hospital 4 days after having the stroke, ran my first mile one week after, and ran a 5K three weeks after the stroke I just completed the halfCmarathon on Dec. 6 and am now training for a 25K in February to mark the one year anniversary after the stroke!
I showed up to my post-op appointment 10 days after the stroke and was told by the doctor I was very lucky to be here and should be in the nursing home with a feeding tube He also told me that I have Fibromuscular Dysplasia of the carotids. After 6 months of taking Plavix to help protect the stents while healing, I had an angiogram that confirmed they were doing their job and I'm now off of the Plavix. I take a daily aspirin, but that's it I have had grand mal seizures in the past. I have tinnitus, and experience quite a bit of dizziness. A small price to pay for a second chance at life!
I am very blessed to be here, and miracles do happen I can only pray my story will help others to know that being diagnosed with FMD doesn't mean you have to stop living!
Melva Buck
I was born into a home with 4 children. I had a much older brother and sister and a younger brother. Much of my memories are a blur.
Continue Reading →
Melva Buck
I was born into a home with 4 children. I had a much older brother and sister and a younger brother. Much of my memories are a blur. My mother seemed to have severe problems with pain, menopause and possibly depression. I became very emotionally bottled within. It seemed as I felt everything but nothing. I do believe that through my childhood experiences, I developed a sure gut feeling for what was important. My onset of menstruation was in sixth grade.
I remember school being very confusing that year. I now believe that I had ADD. I maintained good grades but seemed to hold onto only a little information at a time. During this period, my knees started to slide out of place. There was intense pain and severe swelling after each event. This repeated often, but the last time was while crossing a street. A car slammed on brakes to avoid me, and my mom took me to a doctor. I had knee surgery to correct the muscles pushing on my kneecaps. I spent the summer in casts from the hip to the ankles. The scars from the surgery wrapped around each knee. Through the years, they widened and puckered. They never faded. A few other scars also did the same. With this intense scarring at 13, I chose never to wear shorts again. I am very light skinned. I also noticed during this time that I had multiple visible blue veins over much of my body. My teen years were uneventful other than my periods. They were very painful. I took medications as needed and thought everyone else had the same horrible pains. The other big issue in my childhood was my stomach. Any event that triggered emotions, like my birthday, also triggered my stomach. I had severe constipation issues. It would include a migraine type headache and throwing up. I was diagnosed at 18 with Irritable Bowel Syndrome. The medication for that changed my life. I was no longer trapped by the severe symptoms.
I married at 18. I tried desperately to get pregnant for a few years. I finally succeeded at 22. I always had uneventful pregnancies until the last trimester. My OBGYN discovered that I tended to start dilating early with no pain. I could walk around, shop, or live normally at 7 centimeters with no discomfort at all. I had to be induced with each pregnancy to start labor. I still continued to have some bad headaches, but not to the same frequency as before my IBS medication. I started having higher blood pressure the week before each period. My doctor started me on diuretics for that week which helped.
I chose to be a stayNatNhome mom. I thought my health was excellent other than frequent back issues. If I slept wrong or lifted something heavy, then my back would get intense nerve tingling pains. If my neck was involved then I would feel the neck and headache pain. I started seeing a chiropractor who would do adjustments on my spine. The adjustments always brought immediate relief. I was told by a hospital doctor after a slipped disc incident that I had a curved spine. I went to the chiropractor for years, thinking that the curved spine made my back easily prone to misalignment. My family’s health had never been a big concern. My Dad had an aortic aneurysm, but I thought it was possibly an age related heart defect. In 1992, my older brother, age 46, died from a brain aneurysm. My anxiety soared, since I looked like an identical twin to my brother. My doctor tested me for a brain aneurysm, but mistakenly did the CT without contrast. So all looked great.At 38, I was the proud parent of a 15 yr old, a 13 yr old, a 1 yr old and newborn twin boys. I was very busy but very proud. I developed uterine prolapse after the twin pregnancy. I was told to do frequent exercises to help. As the last children were about to enter school, I decided to get my nursing degree. I enrolled in classes at a nearby college. One day, soon after I had enrolled in my degree, I developed a horrible headache with neck pain. I really thought it was just another bad headache. I kept going until the day I bent over to pick up something off the floor. I felt a wham in the side of my head and I knew that I was about to pass out. I bent my knees to squat on the floor and laid down. I only remember glimpses of memories of a rescue truck and hospital.
I awoke fully in the hospital a few weeks later. I had two aneurysms that had been hemorrhaging in my brain causing the last headache. When I bent over, they had ruptured. The doctor had performed open skull surgery to clip the aneurysms. They had ran a dye catheter to the brain before surgery and noticed that I had funny looking arteries in the carotid. The procedure caused my carotid artery to dissect. They also found smaller aneurysms on the other side of my head. I was informed at this time that I had Fibromuscular Dysplasia.
I spent the next year, recuperating from the surgery. I was placed on antiseizure medications and Coumadin. The dissection had caused a large blood clot to form on my carotid. My doctors always seemed to be unsure about my medical course. They often needed second opinions. I really felt like a freak or at least the only person in the world like this. I guess this phase was denial. At first, I just could not deal with anything else other than getting well and stronger. I distinctly remember the day that I decided to look up Fibromuscular Dysplasia on the internet. There were one or two articles. The article said.. “usually associated with an early death”. This was the anger stage. I cried and I got angrier. I decided to research my options and educate myself.
Through shear luck, I found an online Fibromuscular Dysplasia support group. I saw where there were other people out there just like me. We chatted, we talked, we grew to love each other, and we learned. I started taking research notes, comparing symptoms, and in general accumulating data. This gave me control over my disorder. Because we had our FMD start in different areas, I learned where the other areas could be. I also learned the symptoms. I had no doctor in my area with this knowledge, so I elected to be in control of my own course of medical care. I set up my own preventative care and took in researched data to let my doctors know what to look for. I kept the doctor’s who listened and dismissed those who did not. During this action phase, I found out that I have associated heart conditions, mesenteric artery problems, and renal problems. I also followed a cyst on my thyroid for two years. I felt it one day while driving and made my own appointment to follow up. It was cancer and I caught it before it spread. I have numerous documents that saw it on a scan and said it was probably nothing. During my first visit to a heart doctor, he asked why I was there if I had no symptoms. I answered that I had mammograms every year, but I did not believe that I had breast cancer. He acted like I was ridiculous, but he tested me any way. We found an enlarged heart, mitral valve prolapse, and an enlarged aorta. We found the mesenteric problem after a trip to the emergency room with severe abdominal pain. The doctors wanted to do an emergency angiogram to open the 60% stenosis. I was told that there was a high rate of dissection during the procedure. I just wanted to talk to the support group about it. I refused the angiogram and left. I found out through a vascular surgeon the following week that no angios are needed if only one artery to the intestines is affected. The severe pain was from diverticulosis.
My elderly mother started to have cognitive problems. I decided to move her into my home. She had many various symptoms that seemed odd. I kept asking her doctor the reasons for her odd symptoms, nd he did not know. I decided to look up each symptom on the internet and find a reason. I kept seeing Ehlers Danlos. I finally went to their site and I could not believe it. It was like reading my hole life story. I made an appointment with the NIH study. They confirmed my diagnosis for EDS. I started to study and take notes on EDS. I quickly realized how similar the two conditions were. bout this same time, my FMD group decided to have a small meeting. I flew to Colorado and met several of them. When I entered the room and saw them, I realized that we all probably had a combination of FMD/EDS. Several of them also visited the NIH study. It was confirmed that they did indeed have both.
I now finally began to feel that I fully understood my whole life. I understand the hormonal surges at puberty and menopause and how it related to my FMD/EDS. It explained my knees, my scar issues, IBS, my back issues, and my ADD like symptoms. I understood my visible veins, severe headaches, pregnancy issues, and aneurysms. After menopause, I followed a declining path of high blood pressure, fluid retention, thyroid issues, mitral valve prolapse, dilated aorta, Rheumatoid Arthritis, bouts of Bursitis, and early eye cataracts and glaucoma. I now have a name for all my maladies and that helps a lot. Fibromuscular Dysplasia Society of America has really worked hard to make Doctors more aware of Fibromuscular Dysplasia. We can now find numerous sources of upNtoNdate information nline and at their website. They joined with NORD and The National Kidney Foundation to further spread the data on FMD.
Thanks to this great organization, people with FMD in the future will not be faced with the unknowns that I had to face. I hope they will be able to find up to date information on their computers and Doctors who understand the course of our disorder better.
Patricia Auston
My name is Patricia Auston. I have been a registered nurse for almost 30 years and specialize in Rehabilitation and Neurology.
Continue Reading →
Patricia Auston
My name is Patricia Auston. I have been a registered nurse for almost 30 years and specialize in Rehabilitation and Neurology. I was diagnosed with Fibromusclar Dysphagia 7 years ago at the age of 50.
This is my story.
May 1, 1999
I was sitting in our rehabilitation dining room getting report form the nightshift on my team of patients, when I noticed that my heart rate was racing faster than it ever had before. A coworker asked if I felt OK and I said I wasn’t sure. He then took my blood pressure which was 210/104. This is very high because my normal blood pressure is 90/50 and he said my skin color was awful, blue to be exact. I was then put into a wheelchair and rushed down to the emergency room. The doctors really could not figure out what caused my problems. I am healthy, exercise and fit for my age. After 5 hours and many tests, I was sent home on medication for my blood pressure and told to make an appointment with my primary care doctor. My blood pressure continued to run higher than normal but was controlled somewhat.
May 10, 2000
About one year later, the original problems with my heart rate and blood pressure returned. This time, I was hospitalized for extensive testing to try to find out the cause of this problem. I also knew that with continued high blood pressure, I was at risk for a stroke.I had a cardiology workup, which was found normal. Then a neurological work up which was also found normal. An endocrinologist was called in. He found nothing and suggested nephrology. It was the nephrologist that ordered a MRI of my kidneys. Mind you, this was at the end of a three week hospital stay. Well, they showed me the MRI. It looked just like there was a string of pearls in my renal arteries. The doctor said, he had only seen this one other time and that it was extremely rare. I was very thankful to at last have an answer.The next day, I had a renal angioplasty or ballooning of my renal arteries and was told I would most likely have to have this done about every 5 years. I was sent home on a blood pressure medication and my blood pressure was again within my normal range.
June 6, 2005
I had been doing just fine until out of the blue, the blood pressure problems returned. The doctor was exactly right, 5 years had gone by and it was time for a repeat angioplasty. This time, I reacted to the dye and had an anaphylactic reaction. It was very serious. With medication to counteract this, I recovered.
Here it is November 2007, I have done well, and my blood pressure is controlled again. Of course it is important to eat right, exercise, get plenty of rest and do the entire wellness program. It is very important to monitor my blood pressure as it is really my only sign of trouble. I do not look forward to my next angioplasty because of the terrible reaction I experienced last time but realize that it must be done. Fibromuscular Dysphagia is not a disorder that many people even know about and I think awareness is crucial. Without proper treatment, having a stroke is a very real possibility. If you are affected by FMD, I encourage you to tell your story also. We must educate everyone, including our physicians.
Bruce Tagg
I’m a 52 year old man employed as a Safety Consultant for a major insurance company.
Continue Reading →
Bruce Tagg
I’m a 52 year old man employed as a Safety Consultant for a major insurance company. My wife and I eat healthy utilizing organic products, no red meat and a minimal amount of processed foods. In
addition, we take various supplements and herbs for specific health reasons and general well being. These lifestyle changes were begun over 10 years ago in response to chronic sinus problems and migraines for me and IBS / asthma for my wife. Since the change, migraines have all but disappeared and sinus issues have diminished markedly (my wife’s IBS and asthma are virtually nonIexistent). My energy levels were generally good and while I didn’t exercise per say; activity levels from home repairs, maintenance etc were relatively high. I was rarely sick and didn’t visit our family octor for over 5 years. Overall, I felt that I was in very good health with no history of disease, hypertension, chronic illness or medication use. This all changed one weekend in October 2006.
Due to health problems and repeated hospitalizations of our parents; the past 2 years have been extremely tiring and very stressful. This was combined with increased workload at my job and the renovation of my son’s house. Therefore, when I became extremely fatigued on a regular basis over the past few months, it was caulked up to overwork and stress.
The month of October ended with my being sickened with a “stomach bug”. It was the typical stomach flu type symptoms until the severe sharp pain in my left lower back. It was so severe (although only lasting for several hours), that I went to our family doctor. By this time I had a fever, which would remain with me for over 7 weeks; even after the resolution of the GI issues. A urine test showed some blood and protein, but in minimal amounts. A series of blood work was performed as well as CT scan of the abdomen. All produced negative findings. An ultrasound was performed of the kidneys because he was looking for either a kidney infection or kidney stones. The test was negative and his energies were focused on finding some obscure infection, not an underlying kidney problem. Over the next 4 weeks, I was examined by our family doctor, an Infectious disease doctor, a nephrologist and a cardiologist. They were all focused on some type of infection and continued to order blood work; which never produced any abnormal results. However, they all yielded abnormal results pointing to diminished kidney function. In addition, my blood pressure had risen to 180/120 before leveling off at a low of 140/90; where it remained for the next 8 weeks, despite medication.
In addition, I had a severe, localized head pain located above my left ear and a tingling sensation across the back of my head. At times the pain would extend into my neck. This was definitely different than the migraines I’d experienced in the past. This pain would also persist for over 8 weeks. My left hand trembled to the point where I was unable to hold a glass. There were also infrequent, but severe body spasms. Throughout the next 2 months, the doctors seemed largely uninterested in these symptoms writing them off as just a different type of migraine. At one point, because they were so focused on infection; a spinal tap was performed to rule out meningitis. Even though the MRA showed a possible aneurysm of the vertebral artery, they felt the test was inconclusive. These symptoms would finally disappear in late December after several weeks of lower blood pressure. Multiple MRI’s / MRA’s were performed and only after demanding a triple renal scan (which the doctor felt was totally unnecessary) was the true extent of the kidney function brought to light. They found that kidney function was estimated at less than 50% (subsequent testing suggested the right was 72% & left was less than 20%). Diagnosis was renal artery stenosis and the Nephrologist felt that no follow up action was required at this time because the damage had already been done.
After obtaining copies of the MRA/MRI reports, I noted that they indicated a possible dissection or aneurism of the left renal artery, celiac artery and carotid artery. After discussing these findings with the various doctors, it was agreed (after much prodding) that an angiogram would be performed on the left renal artery with the intention of angioplasty if necessary. There was some reluctance on their part because they felt the risk from the dye was greater than my condition warranted. However, the angiogram was performed on December 19th, two months after first presenting symptoms. Within 10 minutes the angiogram was stopped and the doctor announced that he felt I had FMD even though men don’t get it and nothing further could be done. The presence of the dissection
was never mentioned or discussed.
A follow up visit was made with the Nephrologist and I was informed that he concurred with the diagnosis of FMD. Additionally, he indicated that he had only seen this twice in his twenty years of practice and didn’t believe angioplasty was useful. However he did attempt to locate a doctor with experience in FMD for a referral. Going forward, we would concentrate on blood pressure control and he prescribed various medications and a low salt diet. My next scheduled follow up visit was scheduled in 6 months. While looking for information on the internet to educate myself about FMD; I came across the FMDSA website. My wife contacted Pam with the hope that she might know of a doctor with knowledge of FMD in our area (Allentown, Pa.) since all of the local doctors felt there was nothing to do except watch my kidneys fail. This one phone call turned out to be our Rosetta Stone; for not only did we learn about living with FMD and the need to be pro-active, but I found out about Dr. Olin.
Within one week of calling Dr. Olin, I was in his office and he was going over all of my reports, tests and films. While he (or an associate) spent close to 2 hours with me; the one thing I remember was him saying “You’re in danger of losing this kidney and we need to do something about it.” Finally after 2 ½ months, someone was taking me seriously and was concerned about my problems.
Two weeks later I was back at Mt. Sinai for an angiogram and possible renal artery stent. Unlike the prior angiogram in Allentown, this procedure lasted over 4 hours and resulted in 8 angioplasties. They found not only narrowing and a fairly large dissection, but also a web like partial occlusion. All of the narrowings were corrected and the area of webbing removed. While the dissection was too weak for stenting, the blood flow was restored and blood pressure on both sides of the artery was now the same. The dissection will be monitored thorough ultrasound and MRI to document any changes. It appears that area in question may require bypass at some future point.
An ultrasound subsequent to the angioplasty noted “no significant stenosis” in either renal artery and flow is normal. In addition, my calculated GFR that was 42 in November is now 63. Blood pressure is under control and except for extreme fatigue; I feel really good. Due to the amount of dye received to date, further angiogram of other questionable areas is not advisable. The plan of action is to monitor for 3 months and then have an MRA of the celiac, carotid and vertebral arteries to assess their true condition. At that point a decision will be made whether or not an angiogram of those areas will be performed. My journey with FMD has just begun; I still have to deal with my other questionable arteries and the prospect of living with FMD, HTN, CKD and the possibility of stroke. Eventually the dissection will probably require surgical intervention, but it’s being monitored and hopefully that’s in the distant future. However, I feel like I’m headed in the right direction and I’ve learned a few things along the way….
Lessons learned: 1. I am responsible for my health and I can’t abdicate that responsibility to doctors. 2. I need to pay attention to what my body tells me and not just write off problems
as “just being tired or stress”. 3. Regular check ups and blood work may catch problems before they get to be serious problems, provided I’m proactive (see #4 & #5). 4. Oversee
your medical care, ask questions, get test results, request additional testing, and ask to be referred to a specialist. Don’t be afraid of offending your doctor by asking to see someone
else. 5. Educate yourself about your conditions and tests. This is especially important with something like FMD that very few doctors know about and even fewer have treated. Learn
what the different values on the blood tests mean and follow up with your doctor when needed. It turns out that my creatinine levels were high in 2001, but not high enough for
the doctor to act. I know better now. 6. DON’T accept a nonsensical diagnosis; gray hair is a natural consequence of aging, not a small cerebral aneurysm. This isn’t hyperbole; I
actually had a neurosurgeon tell me that my tremors, body twitches/shakes and possible aneurysm were to be expected with age and there was nothing wrong with me. I found a
new doctor. 7. Most importantly, never forget point #1 Educate yourself and find the right doctor to care for you and your conditions irregardless of distance, insurance, etc.

Nakia Hughes
My name is Nakia Hughes. I am a 333year3old mother of three. After reading stories posted by other FMDSA members, I guess I should consider myself blessed, as I was diagnosed with FMD before having to go through a life long experience of pain and being uncomfortable. In March 2006 I had my third child. It was 4 weeks later that I would get so sick, that I had to sleep sitting up, as I could not breath, was having terrible migraines, and horrible back pain. Of course being a new mom, my family and I immediately blamed this on recent childbirth – not to mention I had him by cesarean section. After two days of unbearable pain, I called my OB/GYN late one night asking if I could have my 6 week check3up 2 weeks early. I went in that next morning. I felt faint, fatigued, and as though I was going to die. Upon taking my vitals, the nurse assumed the blood pressure machine was broken. She tried taking it three times. The doctor finally seen me, and was definitely concerned. He had the nurse check my vitals again. If I remember correctly my BP was 185/111. His office was attached to the hospital where I had delivered so, he asked me to admit myself. My OB/GYN was afraid that I would have a heart attack or stroke.
Upon entering the triage area of the ER, my BP was a whopping 222/165 or something darn close. I remember the top number to be exact. They could not believe I was as strong as I was, although I did not feel as strong. It was the scariest moment I had ever been faced with. I would give anything to trade that moment with another week’s labor and contractions ? Anyhow, thanks to one bright, concerned, and compassionate Dr. at Arrowhead Hospital, we now knew what was causing my inability to find comfort within myself. So to her I say, THANKS As for now, I just left the ER at Arrowhead only to run across one of the many doctors who has no knowledge of the disease, and assumes I can’t move my neck because I have a crook in my neck or I slept wrong. The most frustrating part is trying to explain the pains or symptoms to my doctor or family. Its not cancer or sickle cell, so know one around me understands when I have no feeling in my right toe or that my right side is completely numb and inoperative. I’m mommy, and nothing like this should happen to me, right? I am tired of the pain and other’s inability to understand or want to understand. I am prepared to fight this disease and educate others of its symptoms and effects.
Nakia Hughes Glendale, AZ
Susan Bell
I haven’t yet decided if having a rare disease is a good “thing” or a bad “thing” – but it certainly is some “thing” …
Continue Reading →
Susan Bell
I haven’t yet decided if having a rare disease is a good “thing” or a bad “thing” – but it certainly is some “thing”…My symptoms started, I thought, in my late teens. After years of being clumsy, wearing ankle braces, having multiple dislocations of ankles and fingers (I even dislocated my collar bone at age 2 and broke my arm at age 5) I would now have bouts of kidney problems, irritable bowel episodes and blood pressure spiking all with no known cause. It would always just resolve in time. No consistent medications, mostly diet restrictions were prescribed. I was active and involved in sports and certainly didn’t allow any symptoms to keep me down. However, I never left the house without an “ace” bandage.
After giving birth to my son at 26 my pressure spiked and this time the only resolution was medication. My physician believed it was hereditary as both my Mother and Father were hypertensive.
At 30 my father died of a serious stroke right after his 69th birthday. He was one of 7 children, 6 of whom have died of stroke at or before their 69th birthday. Strokes, gastric problems and irritable bowel were always in my fathers’ family. My paternal grandmother also succumbed to stroke.
At 32 I started to have “on fire” attacks and was diagnosed with coxodynia, bursitis, costochondritis, and back pain. The docs were quick to dismiss it all as early arthritis or some kind of autoimmune disease. Blood tests revealed a positive ANA and a positive rheumatoid factor that were thought to be indicators of “some kind” of disease and I started a nutritional program and years of NSAIDS.At 40 my blood pressure once more could not be controlled and they added another medication and diuretics to try and control it. I had recurrent low belly pain and elevated liver enzymes and after an exploratory laparoscope and endoscope they found numerous “weblike” adhesions throughout my abdomen and “divit like” holes in my esophagus and stomach and an enlarged liver. Again, no diagnosis but “something autoimmune” and they increased all my medication. At about 48 I had another “on fire” experience and my blood pressure went crazy. A reading of 210/120 was a daily occurrence. The third blood pressure medication was added. No physician could explain my symptoms and all were worried that I may have a stroke.
At 51 I had numerous uterine fibroids and very serious belly pain. I had a hysterectomy to try and relieve the pain and my blood pressure immediately went haywire after surgery. They decided to finally do an angiogram which showed renal FMD like a text book picture. I was fortunate to have a cardio/vascular physician who researched the disease and we decided to stent the right renal artery. I now have a perfectly functioning right renal artery with a Herculink stent. However, unlike some, I have never been able to get off any of my blood pressure meds. After my stent placement my pressure dropped for a day or so but never enough to discontinue any of the antihypertensives. I was fortunate to go to the NIH study in 2006 and it was there that I started to put the pieces together. I have confirmed renal artery and carotid artery FMD and spinal stenosis in C2[3, T3[4 with an annular tear, and L2[3[4[5. I share many symptoms of Ehlers Danlos and now understand many of my connective tissue problems. I have some hypermobility and scoliosis and I FINALLY realized I’m not the only one!
I continue to look for answers for myself and others and have tried to use my talents with FMDSA as a volunteer and Board Member. I serve as a Chaplain here in central Florida and have many faith based organizations that I share my time and FMD experiences with. My faith, family, friends and some terrific physicians have gotten me this far and I plan on making it all the way
Rochelle DesRochers, Ontario, Canada
When I was diagnosed with FMD in late 2007, it was unnerving to learn there was little information, treatment protocols, or research available.
Continue Reading →
Rochelle DesRochers, Ontario, Canada
When I was diagnosed with FMD in late 2007, it was unnerving to learn there was little information, treatment protocols, or research available. This lack of awareness resulted in needlessly losing my right kidney and a lengthy hospitalization after what was supposed to be a routine angioplasty in April, 2008.
Fortunately, just a month after I was released from hospital, my husband and I attended the first FMDSA conference (2008) where I met Dr. Jeff Olin, who became my FMD specialist for many years. I also became an FMDSA volunteer at that time, and eventually joined the board of directors. I remember how frightening it was to be diagnosed with FMD when there was no knowledge about how to treat FMD, or what to expect. Since then, many skilled clinical-researchers have researched and contributed a great deal to what we now know about FMD, and that has certainly brought a great deal of comfort. I believe it's vital to support continued FMD research, by participating in studies when possible, and by helping to fund the patient registry by supporting the FMDSA.
Since my event back in 2008, my FMD has been well-managed with medications and monitoring.
I’m always happy to help FMD patients in Canada (or anywhere) to better understand and cope with their diagnosis, and can be reached at rochelle.desrochers@fmdsa.org
Tracy and Alex Toto (mother and daughter with fmd)
When I was 13, I needed a physical to go to camp over the summer.
Continue Reading →
Tracy and Alex Toto (mother and daughter with fmd)
When I was 13, I needed a physical to go to camp over the summer. At that routine physical it was noted that my blood pressure was 180/110. The doctor told my mother that I was probably just anxious and not to worry about it. After a few repeat readings and a few weeks spent in the hospital over the next summer for tests, it was determined that the likely culprit was renal artery stenosis due to fmd. Over the next summer, by now I am 15, I had 2 unsuccessful angioplasties and one unsuccessful renal artery bypass. Lucky for me it was only affecting my right renal artery. My parents at that point got cold feet, and declined any additional surgeries.
A wonderful hypertensiveJnephrology doctor who was just starting his own practice 'found' me and I have been medically managed since then. I have been on vasotec, an ACE inhibitor, since I have been 16 (with brief periods on different drugs during my pregnancies and when I was trying to get pregnant). I carried 2 babies to full term, with just a brief scare of preclampsia at the end of my second pregnancy. My right kidney, after the unsuccessful bypass, started to get smaller, while my left kidney compensated by getting larger and larger. My most recent urine and blood test showed normal kidney function, even with a 3cm right kidney. I have been very lucky. Unfortunately, I had no inkling this could be genetically passed down to my children. A year and a half ago, I was out playing tennis and a sitter was home with my then 3 year old daughter. She was to turn 4 in one week. When I arrived home they were playing in the driveway. I immediately noticed that the left side of my daughter?s face was totally drooping and her eye totally popped open. I feared she had had a stroke and took her straight to the pediatrician. My doctor calmly told me that she had a bell's palsey and that it would go away over time. No need to panic.
Well, I panicked. The next morning I brought my daughter to her ear, nose and throat doctor. She had never seen a bell's palsey in such a young girl and prescribed an MRI to make certain nothing else was wrong. I had to literally strong arm my pediatrician into agreeing with the MRI. She didn't want to subject Alex to unnecessary anesthesia. Ha ! Who could know how many times my little girl would be put out in the next 4 months?
At the MRI, the pediatric anesthesiologist came out after the MRI was complete. He did not want to panic us, but unless we agreed to go directly to the nearest ER he was going to have to call an
ambulance. He explained to us that even under anesthesia my daughter's blood pressure was 200/100.
We went directly to our local ER. There a fantastic cardiologist took my history and explained that she probably had fmd, and that if he were us we should get ourselves transferred to Columbia Presbyterian, in case she had to have surgery or something. What a surreal ambulance drive. Once we were there we had to do the same ER thing and wait until 2am for a room. They did a nuclear scan there and decided that she had unilateral renal artery stenosis. (Which turned out to be wrong). They insisted that the bell's palsey had nothing to do with the high blood pressure and the
fmd and they released us with no medication, just an appt to come back in one week to see the nephrology doctor. Alex turned 4 during that hospital stay.
I could not get out of my mind one line I found on this web site: "and sometimes the severe high blood pressure causes facial palsey in children." I emailed Pam Mace for the name of a pediatric
doctor familiar with fmd in the northeast. She immediately called me back with Dr. Meyer's number at CHoP. I called him, he took my call immediately and we went down there that very day. That day
marked the beginning of a 20 day stay at CHoP. I think I cried one million tears during those 20 days.
Alex underwent 2 CTA scans, 3 angiograms with attempted angioplasties. Thirteen of her 20 nights were spent in the ICU. It was determined that her right renal artery was 75 closed and her left renal artery 90 closed. Alex and I both have the smooth kind of fmd, not the typical string of beads. The angioplasties didn't really do the job and the best they could do was get her blood pressure under control with medicines and send us home with the name of a surgeon in Michigan who might be able to help her.
Alex was sent home on a Sat in mid November and we went to Michigan at the very beginning of December. Dr. Stanley performed her bilateral renal artery bypass (one artery was bypassed, while on the other the affected part of the artery was cut off and the good end reJimplanted in her aorta). After a few scary moments in the PICU, Alex went home 12 days later, right before Christmas. We were overjoyed.
That was when the real trouble began. Almost immediately she had pain after ever meal she ate. I spoke with Dr. Stanley repeatedly. She kept getting dehydrated and ending up in the local ER once a week for fluids because she wasn?t drinking. She didn?t sleep at night because she was in so much pain. I took her to a gastroenterologist who performed numerous tests and eventually told me "it was all in her head." She lost 25 of her preJsurgery weight. I paced with her in my arms for almost 6 weeks.
Eventually I took her to my son's gastroenterologist who called Dr. Stanley's office. He was on vacation but he spoke with the other surgeon in Alex's case. It was known that her SMA was affected by the fmd, but she had never had pain after eating before. Apparently the significant drop in her blood pressure was enough that the blood was no longer getting through her SMA and she had intestinal aschemia. She would have to have another bypass surgery, this time of her SMA. I couldn?t believe it, but was almost joyful to have a reason for her 8 weeks of pain. However, I worried about her physical state. I asked the gastroenterologist if there was any way to 'bulk her up' before her surgery. His suggestion was to get a PIC line put in and feed her with TPN. We did this 2 days later at a children's hospital in NJ, yet another 3 nights in the hospital.February 5th we arrived in Ann Arbor, Alex had a quick angiogram to see if her SMA was indeed affected. It was. She had her next bypass surgery the next morning. This surgery ended up being a reJimplantation of her SMA into her aorta. The surgery was a success. She ended up with a blood clot after the surgery which actually mimicked her pain before the surgery. That took about 2 ½ weeks to clear up. We went home to NJ after she ate her first McDonald's hamburger (yes I cried in Mickey D's).
In May Alex had an MRA of her carotid arteries to see if they were affected by the fmd. It did appear that her brain arteries were affected, not the lower carotids, but up higher in the brain. We elected to go to Boston, to Dr. Scott, for an evaluation. Her brain angiogram in Boston showed normal arteries, she had had a false positive on that MRA. We felt like we dodged a bullet.It is now one year since Alex got home from Michigan and we are a very thankful family. She has had access to the most amazing doctors I think I have ever come across. Both her nephrologist Dr. Kevin Meyers and her surgeon Dr. James Stanley have been wonderful. Not only are they both fantastic at what they do, but also patient with me as the parent (and I don?t let much go without questioning it!) Alex takes a very small dose of vasotec twice a day to keep her blood pressure under control (same medicine as her Mom). She is monitored with blood draws every 3 months and I take her blood pressure every Monday morning. She is now 5 ½ years old and will start kindergarten in the fall. Her SMA is monitored by whether or not she has pain after she eats.
Eventually she will have to have another angiogram. We have decided to go back to Michigan for any additional tests, but until Dr. Stanley says we have to, clinical followJups are enough for me.
Knock on wood my disease hasn?t progressed since I am a teenager (and I am now 39 years old) and hopefully Alex will follow the same path.
My next concern is to do everything I can to help the scientists out there that are trying to find the gene responsible for this disease so that when my little girl goes to have children in 20 years she will be able to screen her embryos for this. It is done for other diseases, so I can dream, right? We can't be sure but my grandmother had unexplained high blood pressure her whole life and my greatJgrandmother died of renal failure in her late 40s. It appears that fmd strikes the women in my family.
Lastly, we spent over 70 nights in hospitals and hotels away from our home trying to heal our little girl. Flying 5 states across the country. We recognize that it is a huge financial burden on parents and since then have worked with the University of Michigan to set up a fund for travel and living expenses for parents who would otherwise not be able to bring their children to Michigan to seek out surgery by Dr. Stanley. We have hit up friends, colleagues and family to contribute to this. Please contact me if you would like to contribute to this fund or if you need financial help. A social worker attached to the University of Michigan Medical Center is charged with determining the use of the money.
Pam Mace
Pam Mace of Rocky River, Ohio, was diagnosed with FMD in 2001, many months after having a transient ischemic attack (TIA) at age 37.
Continue Reading →Pam Mace
Brenda Brondrick
My name is Brenda Brodrick and I live in Olathe, Kansas. Although I had symptoms earlier in my life, my diagnosis begins in 1995.
Continue Reading →
Brenda Brondrick
My name is Brenda Brodrick and I live in Olathe, Kansas. Although I had symptoms earlier in my life, my diagnosis begins in 1995, when during a routine Dr. visit my blood pressure was high. My pressure was too high for a person like myself that was not overweight, ate healthily, taught dance lessons, and exercised regularly.
It took about two and a half years of testing to find out that I have Fibromuscular Dysplasia. A kidney specialist in Massachusetts suggested I have an arteriogram because he suspected this was what I had. After my first visit to the OR I cried tears of "relief" to finally know I had a name to go with what was happening to me. I also cried tears of "sadness" finding out that this disease was "treatable, but not curable." This would be....is something, I have to deal with throughout my lifetime. My FMD is located in my renal arteries, and up to writing this I have had five renal angioplasties. My celiac artery also has some narrowing, but during a recent angioplasty it was discovered that other branch arteries had formed to compensate for this. The human body can be quite amazing when it can protect you in this way.
One of the most painful times in my life was having a renal infarction. After being admitted in the hospital that time, an aneurysm was discovered on the wall of an artery to my kidney. Not knowing if this aneurysm might rupture, or get bigger, or what other problems it may cause along with other symptoms, can be overwhelming at times.
My hope for this disease, is certain tests one day can be as good as those tests that use radiation, and will not expose patients to radiation. Some of the tests I have to have can be harmful over time. In the number of years since being diagnosed, the technology being used for arteriograms and angioplasty has greatly improved. I have had an earlier experience in the OR where I passed out from the procedure, to now having a much shorter recovery time in the hospital after the procedure.
One of the most wonderful things has been finding support through people I have meet through the FMDSA. For the first 12 years after being diagnosed I had never met anyone with this rare disease. After attending an FMDSA conference in Cleveland, it was lifeOchanging for me. I finally could talk with someone who understood what I was going through. It was an overwhelming experience to finally meet people who were "like me". This was very comforting. Many times I feel very alone with this disease, but I know there are other people out there that struggle with the same things I do with FMD.
FMD is something that I have to live with every day. The most difficult part is the not knowing what is going to happen next. Each time I have had angioplasty it seems to work for awhile, then slowly over time my blood pressure rises back up again to dangerous levels, and narrowing in the arteries has to be dealt with too. I experience kidney pain quite often and when I do always hope it's not going to turn into something greater I have learned that my frame of mind can either make me stronger because of what I have, or it can take me down. There are many "down days," but to continue to do the things I love to do, I try to think of why I am stronger because of this disease.
Carrie Kollar
My name is Carrie Kollar. I am a 31-year-old mother of two beautiful children, Nick and Mia and married to my best friend, Joe.
Continue Reading →
Carrie Kollar
My name is Carrie Kollar. I am a 313year3old mother of two beautiful children, Nick and Mia and married to my best friend, Joe. I was previously an ICU Nurse and currently I am leading the IV Safety Team at a St. Louis hospital. I was diagnosed in May 2009 with FMD.My major symptoms started in December of 2007 when I felt ?edgy? and was sitting down eating lunch with my children. I tried talking, but my words got mixed up. I couldn?t recall the name of those bugs that crawl on my windows3 ladybugs. My vision was blurred. I checked for symptoms of stroke and took my blood pressure (BP) 180/110. My BP previously was always 120/80. I thought it was stress and tried to lie down and relax. My BP the next morning was 120/80. Two weeks later I felt it coming on again. My BP was 180/110, but by morning it was back down. I went to an urgent care and they sent me to a neurologist and did an MRI of my head and an EKG but they were both negative. I didn?t have another symptom for a year and a half, except for frequent headaches that I associated with my menstrual cycles.
In April 2009, I got a headache, blurred vision, BP 180/110, went to ER, received an IV blood pressure med, consulted a renal doctor, had another negative CT of my head, and then was started on a daily BP medication. A week later I went to the renal doctor and he said it could be two things: FMD or Pheochromocytoma. He heard a large bruit on my abdomen. He asked me if I had naturally red hair, because when he worked in France, it was common for red heads to have FMD. After the visit, my stomach starting hurting from him pushing on it until it was unbearable. The next day I went back to him, and he took my blood pressure. It was 220/120. He immediately sent me for an emergency angiogram and I was given medications to lower my BP. I had an angioplasty of my right and left renal artery. I had a right renal aneurysm that was not fixed at that time because I had too much dye already. I continued BP medications for 2 days. By then my BP was 120/80 without medication.
In May of 2009, I had severe abdominal pain. An MRI/MRA was done, which showed FMD in my celiac artery. I had previously been diagnosed with reflux 10 years ago. I have had a frequent loss of appetite, pains after eating, and I can only tolerate small amounts of food at one time. I now relate all of these symptoms to the FMD.
In June of 2009, the abdominal pain started again, BP 170/110. I had an angioplasty and a stent placed in my celiac artery. The physician checked my carotid artery, which was negative for FMD. All of my digestive symptoms were gone immediately, and I haven?t had motion sickness (which was severe) ever since.
Both my renal doctor and the interventional radiologist did not understand why I had abdominal pains until?in mid June of 2009, I continue to have episodes of severe abdominal pain that worsened with standing and relieved immediately when I would lie down flat. This was the same pain I had since April, and I also recall these same pains when I was pregnant with both of my children. By 5 months of pregnancy I couldn?t work because of the pains. I thought I was just being wimpy. My BP went up again, but my doctor insisted that it was not the FMD, that it was because of the severe pain that my BP was up. I had a pelvic ultrasound and was diagnosed with ?Pelvic congestion syndrome? secondary to a ?Retroaortic left renal vein? or also called ?Posterior Nutcracker Syndrome?. In other words my left renal vein is compressed between my aorta and spinal cord so it is difficult for blood to flow from my pelvic area to my inferior vena cava, which leads to my heart. All of the blood stays in my pelvic area (ovarian vein) and it has become severely varicosed. I had a left ovarian embolization. The Interventional Radiologist expects that I will have to have the right ovarian vein embolized in the future, but very dangerous because it is not varicosed at this time. I only get the severe pains around my period and I am unable to work a full day when I have the pains.
When I delivered both of my children, my placenta was fibrotically attached to my uterus and it had to be manually detached. It was very painful, even with an epidural, and it took 45 minutes to complete. My OB3GYN at that time did not know why I had that, but I now question if it is related to the FMD.
In October of 2009, my right renal artery aneurysm was coiled and the right renal artery was angioplastied again. My BP was 120/80 without medications. In November of 2009, I had a pulsating stabbing pain on my left lower back. BP was 160/120 for several days. I had an angioplasty of both the right and left renal arteries and arterial pressures showed significant re3stenosis.
My BP has been great since then, but the digestive symptoms have started again. It is very difficult to know what my symptoms are related to. Is it FMD, pelvic congestion, or do I have some digestive issues going on? I fear that I will have to have another procedure soon and each time my scar tissue makes it more painful. I have had a total of 5 procedures since May 2009.
My family has been extremely supportive and caring. I am very fortunate that I have 2 expert doctors that correctly diagnosed me early on. I plan on being a part of any studies related to FMD or volunteer work that I can assist FMSDA.
Shannon Engel
February 9, 2010 turned out to be an evening that I'd never forget. For those of you who don't know me, let me introduce myself - my name is Shannon Engel
Continue Reading →
Shannon Engel
February 9, 2010 turned out to be an evening that I'd never forget. For those of you who don't know me, let me introduce myself @ my name is Shannon Engel, I am 37 years old, have been married for 15 years and have two great kids. I live an active, healthy lifestyle and had recently got involved in triathlon training. So when I started getting chest pains that night, I couldn't figure out what could be the cause of that kind of discomfort and went to bed (seriously). I woke up feeling a little better that next morning but I have to admit, when my left arm kept falling off the steering wheel while driving to work, I thought it was more than a little odd but I still couldn't rationalize what was happening to me. It wasn't until I got to the office and began working that my chest pain came back and I decided it was time to walk myself next door to the West Lincoln Memorial Emergency Department.
I remember Dr. Buller introducing himself to me after reviewing my chart and explaining that I would be going in for an angiogram. It was during that time Dr. Buller could see that there was a healed dissection of a larger artery and the dissection of this second artery is what caused the heart attack. He checked my kidney and didn't see anything of concern and was then diagnosed with coronary FMD. Fortunately for me, Dr. Buller is a specialist in FMD and had recently moved to Ontario from living out west and just happened to be on call that day. It's through careful monitoring, medication and reduced physical activity that I am (sometimes reluctantly) learning to live with this disease. What I find most difficult now is mentally being more than ready to go back to my lifestyle of running, swimming and biking but realizing my physical limitations.
With these kinds of odds on my side, I would have preferred to have bought a lottery ticket but I can honestly say that there is not a day that goes by that I don't thank God for my good fortune. I just celebrated my second 'birthday' on February 9, 2011 and hope for many more!
Sincerely,
Shannon Engel
Barbara McFee
I am a Registered Nurse who also served as a Coroner for many years. I have a Master's degree in Administration.
Continue Reading →
Barbara McFee
I am a Registered Nurse who also served as a Coroner for many years. I have a Master's degree in Administration. My diagnosis of FMD of the right renal artery was made when I was 66 years old which is rather old according to all the literature that I have read.
I was diagnosed with hypertension in my late 30's and took one medication for many years. I never smoked, drank alcohol, always exercised and have been on a balanced diet of chicken, fish, whole grains, fruits and vegetables for many years. My mother had hypertension.In 2001, I was in a car accident where my new car (10 days old) was totaled as I was TLboned by a man running a red light. Several months later as I was preparing to leave for Canada to help settle my mother's estate, I was making a left turn on a busy intersection and all of a sudden, I became dizzy, shaky and thought I was going to pass out so I stopped my car and someone called an ambulance and I was taken home. I went to a physician who diagnosed me with a panic attack, put me on tranquilizers and so I thought that I had a problem with driving and perhaps reacting to my mother's death.
I continued to function as an R.N. working long hours until in 2005, I collapsed with a blood pressure of 230/110. I had 7 hospital admissions with diagnoses of dehydration, pulmonary embolism, anxiety, fatigue, etc until the physician who I worked with suggested " why don't they check your kidneys". The ultrasound showed right renal artery FMDL severeL and the renal angioplasty was performed. I was so weakened by the escalating blood pressure and anti-hypertensive medications that I spent 57 days in a nursing home trying to walk and cope with the side effects of the medication. All rehabilitation patients have psychiatric consultations and when the psychiatrist came to see me and asked if I would talk to him, I replied "sure, if you were misdiagnosed 7 times prior to getting treatment for a medical condition, would you feel crazy?" He laughed and replied "well, your sense of humor is still intact".
I spent the next 5 years with a very few blood pressure elevations and than in 2010 at Xmas time I was back in the hospital with uncontrolled hypertension. I was reassured that I did not have FMD again but my cardiologist ordered a CAT scan and there is was L on the right and the left side now. In February of 2011, I had a right renal angioplasty with the radiologist using a " cutting balloon". The left side did not have a stenosis so was left alone. Two weeks later the symptoms of burning in the chest wall, escalating hypertension, and even numbness in my legs occurred. I again entered the hospital and had a cardiac angiogram and a 3rd renal angioplasty. My blood pressure is still not stable on Toprol XL 50 MGM BID, Lisinopril 20 MGM BID, Norvasc 10 MGM DAILY, Hydrochlorazide 12.5 MGM DAILY, Clonodine 0.2 Mgm Patch weekly and Clonodine 0.2 Mgm prnLusually 3 times per day.
Next week I will return for a procedure to evaluate the circulation in my right kidney. Many small vessels are involved so the outcome may not be what I want to hear. I am determined to become stable again and enjoy my independent life style for a few more years.
The biggest challenge is finding a physician and hospital staff who actually understand the disease. I have been busy passing out Pam Mace's wonderful article to health care providers in the hope that they will educate others. In 50 years, I never encountered a patient with this diagnosis. This website is invaluable allowing patients to share their experiences.
Tracey Renae
I woke up on the morning of March 10, 2011 with what I thought was a bad migraine.
Continue Reading →
Tracey Renae
I woke up one morning in March of 2011 with what I thought was a migraine headache. I got in the shower and started getting ready for work. I was a kindergarten teacher. I had to get my own kids (then 11, 9, and 6) up and ready for school, too. Somehow, I got dressed and made it down to the kitchen with the kids. As I was walking toward the refrigerator, I felt dizzy so I sat down. My daughter asked if I was okay and I told her not to worry, I just had a migraine and would be fine. Then I started to feel nauseous. I don’t remember how I got to the bathroom, but managed to do so and sank to the ground. The room was spinning. My daughter told me it was time to leave and I told her to get her brothers in the car. I guess I could go without breakfast today. She then told me I was not making sense. She said she thought I was too sick to drive and she told her brothers not to get in the car. I couldn’t even stand up. She asked me if she should call 911 and I repeatedly told her no—it was just a headache. I don’t remember anything else from that morning.
My daughter did call my mom. She told my mom that I had never been sick like this before and that I couldn’t drive or go to work. She told my mom that she and the boys were ready for school and they still had time to catch the bus. I usually dropped them off at before school care on my way to work. My mom drove over right away. She found the kids standing in the rain at the bus stop. Before they got on the bus, my daughter told my mom that she left the front door unlocked and she could find me on the bathroom floor, talking funny. My mom rushed down the street to our house.
I do not remember any of this happening. One side of my body was so weak and useless. My mom immediately called 911 when she saw me and the paramedics where there within minutes. I spent the next week or so in the hospital.
I was initially treated for stroke like symptoms in the ambulance and taken to the stroke unit at our local hospital. My breathing soon became labored and they had to intubate me. I also had CT and MRI scans, x-rays, EKG’s, lots of lab work, and a spinal tap. They told my family that I did not have a stroke and they admitted me to the neurology ward. I continued to be in severe pain and lost consciousness after extreme dizzy spells a few more times while in the hospital. They kept running tests and telling my family that everything was fine.
After a week in the hospital, I was discharged to go home and was told that I had complex migraines and that I should look into getting some psychiatric therapy if life was “too much” for me. I still had a headache when I was discharged and was still so very week. I couldn’t walk without help. My family was surprised that I was being sent home in this condition with no real answers about what happened.
A few weeks later, I was able to meet with a neurologist that a good friend recommended. Until then, I had been forced to see neurologists that my insurance company told me to see in order to qualify for short term disability. I met with my friend’s neurologist as a second opinion and he spent 2 ½ hours with me and went over all of the hospital reports and testing that had been done. He did not just read the reports, he also looked through each scan. That’s when he saw it.
My right vertebral artery had dissected due to a rare arterial disease called fibromuscular dysplasia (FMD). He showed me the CT scan. My vertebral and carotid arteries looked like strings of beads. He also told me that I was very lucky to be alive. I may not have had a full-blown stroke, but I did have a “mini stroke” or transient ischemic attack. I was misdiagnosed at the hospital. I was lucky to be alive and lucky to have found a doctor who had actually heard of fibromuscular dysplasia. He had my hospital chart amended and ordered further testing that showed I also had fibromuscular dysplasia in my renal arteries as well. He also became my neurologist until his retirement many years later.
Now, all of my family knows the signs of a stroke and they all know when to call 911. Insurance denied my short-term disability because their doctors had never heard of fibromuscular dysplasia and continued to believe the complex migraine diagnosis. I am no longer teaching kindergarten, but I am grateful to be alive.
Cristin Scali
My name is Cristin Scali, I’m 51 years old and I’m from Long Island, New York. I was diagnosed with renal artery FMD.
Continue Reading →
Cristin Scali
My name is Cristin Scali, I’m 51 years old and I’m from Long
Island, New York.
I was diagnosed with renal artery FMD December 2017 after suffering
two years with undiagnosed symptoms. My nephrologist had me take every test possible and finally figured out it must be FMD. I was both relieved and sad at the same time not knowing what was to come in the future for me. But he found me a wonderful cardiologist and the
two of them made up a plan and three days later I had bilateral renal
angioplasty. If it wasn’t for Dr. Barbato and Dr. Deutsch I never
would’ve known what truly was wrong with me. But now that I know what I have and found your wonderful FMD society “club” I can
spread the word. Having all the valuable information on the disease
and what tests to take is so helpful. Thank you for all you do and
good luck to all my fellow FMD patients!
Lori H
It was a sunny October day, and I was heading to the Hospital to meet with a Cardiologist to review the findings from my MRI.
Continue Reading →
Lori H
First off as I tell my story you will realize I think in run on sentences please don’t be alarmed not brought on by FMD.........and so my story begins.
It was a sunny October day, and I was heading to the Hospital to meet with a Cardiologist to review the findings from my MRI for the challenge I had been experiencing with lifting my arms above my head. I found in yoga and spin class with light weights anytime I had my arms over my head I would start to sweat and feel nauseous it would be at least an hour before recovery. I had been for an MRI a few years earlier for extreme frontal headaches and head pressure, that I now believe was my first major symptom for lyme disease.
Of course at that time they told me I was fine. So with having an MRI prior in my mind I thought again this is linked to lyme disease, and they will find nothing and think it’s all in my head........well close, actually my neck.
The cardiologist greeted me if you could call it that with, “did you know you are high risk for aneurysm?”. Fine thank you, and you, wait WHAT? It was at that moment I was told I was a member of the FMD club ....and then the fog set in. That which slowly removed me from reality and all I could hear was my breathing. Familiarity lingered on the word aneurysm as I know how that story goes, I had experienced it within my immediate family. The only words that I heard were my own,”am I okay to just leave?”, to the response, ”well you made it this far”. Did she realize her words were now deep rooted in my memory along with an incidental finding.
What happened next...well, immense fear, “sorry we don’t know much about it” and feeling very alone. My mind or sense of reality went right out the window. My FMD is in my carotid arteries so I thought okay no head or neck movement. I admit, so much so that, I would sleep like a solider who was guarding the palace. I can promise you my neck did not move but my back was killing me. Also, odd when you try not to move your head and neck you hold your breath...try it. Yeap not a good initiation into the club. Then my walking became very methodical slow and calculated so I didn’t disturb any one of those pearls on my necklace. As I said this is my story and honestly I want to be in the over 85++ club so I was scared. I immediately lost my appetite and ate small portions of selected food documented to not clog arteries. The only medical advice was to keep stress at bay and blood pressure in the normal range which at that time in my life was beyond a challenge.
Then came the engagement with the Specialist community. Highly educated and respected experts of their field but not quite versed within the FMD world. Such a small number of us patients, no grants to support study and their dance cards are beyond full. I was told by one if I had presented at 30 something he would have been more invested in following me closely. Hmmm, let’s see with one FMD conference under your belt, yeap thanks for that, this not so “spring chicken” is not putting all her eggs in your basket. I wonder what google search deems the age limit is supposed to be about caring for your longevity? So, the road to date has had a few potholes. However, it would not be fair if I did not acknowledge one amazing Specialist who is the Chief of Vascular surgery. He was honest in what he knew and his dealings to date and when I asked if he would see me yearly, he said yes.
Gabriela Aparicio
Hello my name is Gabriela and I am 48 years old, I live in Santiago, Chile. I really don't know when my FMD started.
Continue Reading →Gabriela Aparicio
While putting on my makeup getting ready to go out to dinner I noticed my right eye was dropping. The
following day I saw my Internist who sent me to my Neurologist. We spent most of the appointment talking about my migraines which seemed to be increasing. He had suggested I have an MRA because of the drooping right eye, but the conversation had gone elsewhere and I was about ready to walk out the door when he said, “Why don’t you have that MRA”. The following morning I had the MRA and nothing could have prepared me for the call from my Neurologist a couple of hours later. I was told they did think I had an aneurysm and needed to have a CTA the following day. My parents had just moved to a Retirement Home in Atlanta, my daughter was scheduled to deliver my second grand son two weeks later and I was starting a
new Interior Design business. Life could not have been better.
The CTA confirmed the aneurysm and I was sent to a Neurosurgeon for further evaluation. That resulted in a Cerebral Angiogram. The recommendation was to do nothing about the Aneurysm. In fact they actually found two, but they were small and highly unlikely to rupture. As so many of us with FMD often say, “I felt like a walking time bomb.” What I didn’t know that day
was that they found much more.
Six months later while reading a book in bed stroke symptoms
began. The right side of my face suddenly went numb, I got up and realized I had a very hard time walking to the bathroom. I tried to google “stroke symptoms” and my right hand was uncoordinated and I had a hard time doing it. Living alone I had not spoken all night so didn’t know until I called my daughter that my speech was very slurred. Once I heard myself talk I made the call to 911. I was very puzzled since I didn’t have any risk factors for stroke. After being diagnosed with a TIA and spending the night in the hospital I decided I needed to get that Angiogram report. I got quite a shock when I saw that I had some disease called Fibromuscular Dysplasia in both Carotid and Vertebral Arteries and also in my Petrous, Cavernous and Supraclinoid
segments of my Internal Carotid Arteries. Then there was more.....
The CT scan they did after the Angiogram showed that I had encephalopathy in my left frontal lobe from previous ischemia.
Rose
Well it's been 3 1/2 months since my stroke and by the grace of God I feel fine.
Continue Reading →Rose
I am 56 years old and I was diagnosed with FMD in January after having a stroke.
I have been suffering with migraines most of my life and getting treated the last 8 years with medication and botox injections. April of 2021 I had an awful case of Covid. I literally was vomiting for almost 2 weeks. I never felt myself after that. As the months went by I noticed many weird symptoms. I had brain fog, confusion, memory loss, lightheadedness, tinnitus in my right ear, and the occasional whooshing sounds. I was told I was a "Covid Long Hauler".
Later on in the year the migraines got worse, especially in December. The migraines were more frequent and they were accompanied with pulsatile tinnitus. This past January 2nd is when I realized I was having a stroke and my husband called 911. I am very fortunate to live in an area where they reacted very quickly and even sent what's called a "Stroke Ambulance Unit" to my house within 5 minutes. They were incredible. This ambulance was equipped with a CT scanner and telehealth neuroradiology services linked to Stonybrook Hospital. They immediately got an IV in me, administered dye and were able to perform a CT scan angiogram. That's when it was determined that I had a dissection in my right carotid artery. I was rushed to Stony brook hospital and seen by Dr Fiorella. Within the next 20 hours additional tests were performed including MRI, MRA, and standard Angiogram.
Final diagnosis was Fibromuscular Dysplasia. Dissection of the right carotid artery with a blood clot and stenosis of the left carotid artery. As of now I am on Eliquis and aspirin and will be monitored carefully with MRI and MRA again this month and repeat angiograms periodically.
My personal opinion, I believe I have always had FMD and maybe from all the straining of the vomiting from covid, I must have torn the carotid artery. So far that has been my journey with FMD. I also want to mention that after speaking with family members, it was brought to my attention that I have a cousin that lives in Italy also was diagnosed with FMD 25 years ago. Her case, however, has been much worse. It has affected her renal, carotid and vertebral arteries.
Thank you for letting me share,
Rose
Adolescent FMD
Kelly Paprota
I was 17 years old when I was first diagnosed with FMD. I was very active—played on my school’s soccer team.
Continue Reading →
Kelly Paprota
I was 17 years old when I was first diagnosed with FMD. I was very active—played on my school’s soccer team, was Class Treasurer for Student Council, sang in my high school show choir, and played violin in the orchestra. As far as I knew I was healthy…I didn’t really think much about my health to be honest. My mom is an RN, and she was good about keeping us on track with routine checkups and things. I figured I was covered!
The only complaint I had was severe headaches that occurred about once a week. My doctor said they were migraines, then he said they were tension headaches…none of the medicine they gave me for them did any good so I just learned to live with them. In the spring of my junior year of high school, Student Council hosted a blood drive in the school’s gymnasium for any student that wanted to donate blood. I decided to donate, even though I felt a little queasy at the thought of it. Those of you who have donated blood will remember that you start off in two little booths, where they do routine checks on your vital signs and your blood iron levels to make sure everything is ok for donating. One of the nurses put the blood pressure cuff on my arm, waited a minute, and said “Hmmm, that can’t be right”.
She pumped up the cuff a second time, and again shook her head. She called for another nurse to come over and give it a try. The second nurse pumped up the cuff again, waited, then exclaimed “What?? This little thing?? Hmmmm, I just don’t know…” The nurse then told me that for some reason, my blood pressure was too high today for me to be able to safely donate blood. She said it was probably some sort of fluke, and that I could come by their office later this week if I still wanted to donate. I shrugged it off, having never been told my blood pressure was high before. I was more upset that I didn’t have an out for soccer practice that evening than anything else My mom was out of town until late that same night, and she came in and woke me to say hi when she got home. Sleepily, I hugged her and told her welcome home. Then, I said, “Oh, and by the way…the nurses at the blood drive today said something about having high blood pressure…I’m not sure what that’s about.” She immediately got her own cuff out of the car to see for herself. (At the time, she was a Home Health nurse so the family car was pretty much a mobile hospital.)
She checked it and calmly said, “Change your clothes; We’re going to the hospital”. Of course I protested…I mean it was midnight, I was in my pajamas, and I felt totally fine She insisted. She tells me now that my blood pressure was upwards of 200/140 at that time. We got to the ER, and were seen by the triage nurse. My mom shared her concerns, and the ER nurse checked my BP with some sort of machine there in the nurses’ station. I remember that it started beeping loudly both times she checked it (a warning or error beep?). They put me in an ER room, hooked me up to some machines, and monitored me for a while. They admitted me after a few hours, when my BP dropped dramatically upon standing and I almost passed out. Over the next few days in the hospital, I had lots and lots of tests done to help the doctors figure out what was making my BP so high. I was very frustrated all this time, because I felt totally fine and couldn’t understand why I needed to be missing school and other activities. The doctors were frustrated too, because all their tests kept coming back normal.
I had MRI’s, CT scans, CAT scans, blood tests, you name it. On the fourth day, my doctor came in to tell me that I was being released since they couldn’t find anything wrong. “It must be just essential hypertension”, he said. My mom was very upset at this decision, and knew this couldn’t be right. I just wanted to go home. Then, about 20 minutes later, my doctor came back in the room and said “Never mind, we just got the results of your renal scan back and we need to run some more tests”. They did more renal and arterial scans, and gave me the diagnosis of FMD the next day. Of course I hadn’t heard of it, and my mom hadn’t either. The doctors went on to tell us that my right renal artery was 90% occluded (blocked), and my left was about 20% occluded. This was what was causing my high blood pressure, they said. They also told me this was the likely cause of my severe headaches, and that I was lucky I hadn’t had a stroke. These were sobering words, for sure. The treatment the recommended was to do a “routine angioplasty” on the right artery to open it back up for blood to flow through. The left was not severe enough to warrant treatment. I agreed to the procedure, and they prepped me for it. I remember the doctor quickly giving me his spiel on what they were going to do during this and how it would all work right before going in for the procedure. He told me I would be conscious, because I had to be able to hold my breath and move slightly if needed for them to get the wire where it needs to go. I told him I understood, and we were ready to go.
Right at the end, the doctor added, “This NEVER happens, but I have to tell you just in case…in some cases during an angioplasty, the artery can tear…and we do have a backup surgical team on call to go in and repair that tear if that were to occur. But it never happens, don’t worry.” And then I was wheeled in. The angioplasty itself was quite a strange experience. It’s an interesting sensation to have this little wire poking around inside your body…and a big screen above you where you can see it moving around in your arteries…and doctors talking about you to each other as if you aren’t awake yet you are…its very surreal. Finally, they got the wire into position and inflated the tiny balloon. I heard them say they weren’t entirely satisfied, so they were going to inflate it a second time. All of a sudden, an indescribable gut`wrenching pain ripped through me, and I heard all sorts of confusion and shouting of orders from the doctors.
There was chaos that to me seemed like hours…I remember screaming in pain and not understanding what was going on. A nurse told me that my artery had ripped during the procedure, and that I was going into emergency surgery because I was bleeding into my body cavity. I thought I was dying. I might have been. I cried for the anesthesiologist that they told me was coming….I remember asking over and over when he was coming in because I wanted the pain to stop. Later I was told this all happened in less than 10 minutes, but it felt like a lifetime. The next thing I knew, I woke up in ICU struggling to breathe. I had a respirator tube in my throat and I didn’t realize it was breathing for me. I think my whole family was in the room, too. I was confused at first, but they told me what had happened.
My artery had “shredded” during the procedure (“That NEVER happens, don’t worry”…) and I was bleeding internally. They had rushed me into emergency surgery, put me under and made an incision from the bottom of my sternum all the way down my abdomen, stopping 3 inches below my belly button (they went around it ). Then, they made an incision on the inside of my right thigh. They grafted a piece of artery from my leg onto my right renal artery to replace the portion that had torn. They stapled me back up again, and I woke up a while later in ICU. The recovery from this emergency surgery was painful, both physically and emotionally. I was in the hospital for another 8 days following the emergency procedure. I was fed through a feeding tube for the first few days, and I lost 13 pounds (when already thin) and looked completely emaciated by the time I went home. As a 17 year old girl, you can imagine the horror and shock I felt when I saw my abdomen stapled all the way down for the first time. Also, it was painful to stand up straight and walk since they had cut through my abdominal muscles.
All of my many visitors from school were given the task of making me walk around the hospital wing with them, holding onto my IV tree, to help the healing process. Even though it was a near`death experience (the doctors admitted afterwards that they weren’t sure what the outcome would be), the solution that had ultimately occurred ended up being the best treatment possible for my FMD. Now that I have a graft leading into my right kidney, the FMD can’t affect that area again. As for the other side, I am keeping an eye on it. I do have to take medication every day for mild hypertension, however.
My blood pressure returned to normal for a few years, but then started staying at about 130/90 consistently. It is well controlled with a low`dose ACE inhibitor and regular exercise. I no longer have severe headaches. Even though what happened to me was pretty traumatic and also painful, I can still say I am glad things turned out the way they did. It gave me a better appreciation for my life and my body, and I don’t take those things for granted anymore. I wouldn’t even want to get my scars removed if I could, because I see them as fond reminders of a hard part of my life that made me stronger. Few people with FMD will experience what I did, but I hope that reading my story will prepare them for the worst… the part that doctors like to say “NEVER happens”.
Jeffrey Sweeney
Hello, my name is Jamie Cribb and I am the very proud grandmother of Jeffrey D. Sweeney age 14.
Continue Reading →
Jeffrey Sweeney
Hello, My name is Jamie Cribb and I am the very proud grandmother of Jeffrey D. Sweeney age 14.
January 17th, 2010 our Jeffrey was outside sitting with friends when he became dizzy and started having a headache. Jeffrey told his friends that he was going home and when he started to get up his left side would not
function, in an attempt to get up again he fell more to the left side and also dislocated his left shoulder. At the time his speech was slurred as well per his friends.
The friends ran in to tell his dad who right away picked him up and took him to the ER, the staff immediately placed him in immobilization thinking that he had hurt him self while on the trampoline. He was placed on a monitor, IV was started. He had ct scans and still no answer as to why a healthy young man had left side paralysis. He was taken by EMS to the Medical Center of Central Ga. Twenty six hours later, my daughter called to let me know that our Jeffrey had had a stroke. Still it is hard to imagine.
In the first week ,he started moving his left leg, but not his arm. He started rehab there and was then sent to Scottish Rite for further rehab. Today our precious boy can walk, but has a brace in his shoe because his ankle only has minor use and he can only move his great toe and that is with a lot of work, as to his left arm he can move it some. Can not pick up anything with his arm.
This summer he started back to school and is playing ball again with a team through the board of education. This team is called the "Sharks" and is only for children with physical disabilities and they all play in wheel chairs.
Jeffrey tells us that his life has changed and he has to change with it. This young man has shown us a lot of strength and courage. He has worked hard to get to this point and we are so very proud of him. When I look at my precious grandson, I see a new young man, but still a child with hopes and dreams. His neurologist has given him permissin to obtain his learners permit this month as he will be fifteen. He told me, "you know grandma when you come over to get me, I will drive you home. Makes me a little nervous, but if he has the courage, so do I.
This is but a small story of our Jeffrey, this is not all he went through. It was hard for him and he has walked a very hard road and learned a hard lesson about life, but we are so thankful to God that he has allowed us to keep Jeffrey. Now we pray that his life will be full of happiness and no more strokes. What a wonderful young man he is. May God continue to bless him and others who are dealing with FMD.
Today I try myself to teach people about FMD. Being a nurse this is something myself that I have never seen before and read all I can. I hope more will become aware of this and help to find a cure. Many Thanks for reading the story about our Jeffrey.
Jamie&Cribb
Very Proud grandmother
Pediatric FMD
Ayaana Daruka
Hi! My name is Manisha Daruka. I live in Jaipur in India. I have a 5 year old son, Ahaan, and a 1 year old daughter, Ayaana.
Continue Reading →
Ayaana Daruka
Hi! My name is Manisha Daruka. I live in Jaipur in India. I have a 5 year old son, Ahaan, and a 1 year old daughter, Ayaana. Neither my husband nor I have any family history of FMD or any stroke related disease, but my daughter Ayaana has been diagnosed with FMD recently. Till the age of 7 months, Ayaana was perfectly healthy and a normal kid with no symptoms of any kind of illness.
On 12th April 2011 when Ayaana was 7 months, she was cranky and irritable all day. We consulted her pediatrician who suggested it might be a stomachache or urinary infection, which is quite common at that age. Two days after that Ayaana had convulsions. We rushed her to hospital, and after inspection doctors told us that she had a stroke, which affected the right side of her body. There were no pre stroke symptoms. The stroke was confirmed by the CT scan, which showed infarcts on the left side of the brain. The doctors at that time could not diagnose the reason for the stroke. For the next 2 weeks she was playful and improving physically with physiotherapy.
After 20 days, Ayaana was very irritable and crying all day. We took her to the doctor but they suggested we should wait as they didn't see anything specific. Later that night, when I woke up to feed Ayaana, I noticed her left limbs were not moving. Doctors confirmed another stroke, this time on the other side of the brain, the right side. The brain MRI and MRA studies revealed an acute infarct in right occipitoparietal frontal. Jaipur, being a small city with no advanced medical facilities, we were suggested by the doctors there to move Ayaana to another hospital in Mumbai.
Ayaana was admitted to the hospital in Mumbai. After running various tests and scans, investigations showed B/L internal carotid artery stenosis and marginally thinned out MCA. She was also found to have baseline high BP above the 95th percentiles. Hence renal Doppler was done, but were normal. Rheumatologist was referred to rule out the possibility of vasculitis. PET CT for vessels showed no activity. As the investigations were not so conclusive doctors decided to give a 2-week steroid trial.
On 23rd May 2011, Color Doppler examination of the Arterial System of both upper and lower extremities was done. In the lower extremities the left PTA was found tortuous with intimal thickening and beading. As for upper extremities, a significant stenosis (>75 % diameter reduction) was seen in distal left axillary proximal brachial artery. On the right side there was an area of stenosis (>50% diameter reduction) in the axillary proximal brachial artery.
On 2nd June 2011, we got another renal Doppler done. Investigation showed both the kidneys were normal in size but the intrarenal arteries on both sides showed mildly raised velocities (>200 cm/sec) with borderline high RI values. A color aliasing was seen in proximal renal arteries bilaterally suggesting proximal segment stenosis.
On the evening of 2nd June, Ayaana got very cranky and we rushed her to the hospital where it was found that her BP was 177/102. The interventional Radiologist at the hospital reviewed her MRI and MRA films and decided to do balloon angioplasty of both the carotids to avoid further stroke.
On 4th June 2011, DSA was done s/o FMD involving carotids & left renal artery. Angioplasty was done for the left ICA.
On 8th June 2011, just 15 minutes before she was to be taken for a second plasty, Ayaana collapsed with left focal convulsion following a small dose of IV Midazolam. She was intubated and a short CPR of 15 sec was given to her. After this collapse MRI + MRA showed a new infarct on the right frontal periventricular white matter, focal stenosis in the proximal right cervical ICA. She was kept ventilated for 48 hr.
On 10th June 2011, second balloon angioplasty for the RICA was done. Renal films taken at that time did not show any remarkable renal vessel narrowing. Decision was made not to plasty the renal vessels at this time. No stents were used in both the angioplasty citing her age.
Due to the repeated punctures on the right thigh for the Angioplasty (puncture was always made on the right because there was a higher stenosis in the left leg), blood flow reduced considerably in her right leg. Just by touching I could feel her right feet colder than the left. Doctors suggested that this is a common phenomenon after punctures and will improve with time.
She was discharged after a few days and put on regular physiotherapy. Her blood pressure continued to be of concern and we were advised to check it at least 3-4 times a day. She was put on labetalol, ACE-inhibitors and amlodipine. Her BP slowly came back to the target of 120 systolic with these medicines. But for the last one month it has been rising again and doctorsadvise that she is already on maximum doses of these medicines. Currently she averages 160 systolic. We are scheduled for another CT Angio this week to see if there have been any developments on the renal artery stenosis. The last carotid Doppler revealed a mild narrowing in her left carotid compared to the state after balloon angioplasty, but doctors suggest its not threatening right now.
Doctors here are taking Ayaana's case as it comes. Ayaana is 14 months old now. They say that at her age, the disease can be more aggressive than in adults, though we are hoping that Ayaana grows up to be a normal kid. She is always smiling and happy like nothing has ever been wrong with her. I am very proud of her. Her smile gives my family and me a lot of strength and hope. I am waiting for the day when she walks and talks to me.
I hope story of Ayaana helps others and those who read her story can probably help her too.
Jordan Diggs
She's a giggly girl. She says she's funny too, knows a lot of jokes. But when you ask her to tell one.
Continue Reading →
Jordan Diggs
She's a giggly girl. She says she's funny too, knows a lot of jokes. But when you ask her to tell one, she just giggles instead. The giggle and a big, toothy smile cover up that Jordan Diggs, 9, has been sick most of her life.
She has fibromuscular dysplasia. The Web site ED medicine.com defines the condition as an “arterial disease of unknown etiology typically affecting the medium and large arteries of young to middleDaged women.”
The condition is rare, according to Jordan's parents. It affects arteries in different parts of the body. In Jordan's
case, she has arteries that look like a string of beads in her kidneys and in both her small and large
intestines.
If the condition moves to the carotid artery, it can cause different kinds of strokes. How serious is it? EDMedicine.com says in the United States, the condition is found more frequently by autopsy than by other means. The bubbling of her blood vessels decreases blood flow throughout the body and causes high blood pressure, which is how the condition was discovered five years ago, when Jordan was 4.
Her blood pressure hit 299/148 at that time. She was sent to Piedmont Medical Center, but the Rock Hill hospital sent her home and told her to come back if she didn't feel better the next day. Jordan's mother Emily said the family took Jordan to Dr. Sam Stone after coming back, and he sent Jordan to Carolinas Medical Center. Her main problems now are focused on her intestinal arteries. She gets nauseous and doesn't want to eat or drink, so she suffers from dehydration frequently. She doesn't like to say how she feels when she's sick. She remembers the gas and feeling “funny” when she was anesthetized way back when. Emily Diggs remembers the emergency staff at CMC having to give her daughter an intravenous drugs to get her blood pressure down. Doctors were afraid the girl had had an aneurysm until they took a look at her kidney veins.
Jordan has had angioplasty a couple of times on her renal arteries, the ones in her kidneys. She is young, and those arteries haven't fully grown yet. The ones she has had worked on are just big enough to allow the smallest “balloon” insertion to be put in to open up the arteries.
She's had balloon angioplasty done to one artery in her left kidney and to two arteries in her right. She's got to wait until she's grown up more to do other angioplasties on her intestinal arteries. She can go to school with her friends, but she often has problems when she doesn't eat and drink enough. So she has been in and out of the hospital all her short life. The condition can be life threatening. She goes for routine exams every four to six months. It's been almost a year since she was hospitalized for dehydration. She admits, with a giggle, that she didn't have any problem eating or drinking last week.
The MakeDADWish Foundation, an organization that grants the wishes of children with life threatening medical conditions, accepted an application from Jordan's family, signed off on by her specialist in Charlotte, to grant Jordan's wish. She wanted to go to Disney World, her mother said.
She got to do that, and more. The foundation paid for a week in Orlando, where the entire family, Jordan, her father Bill, Emily and Jordan's 11DyearDold brother Tyler, they took in all the attractions D Universal Studios tour, Seaworld, GatorLand. Jordan got to meet her favorite princess, Cinderella. It was a special week. She didn't know if she was the only kid in her school who got to go to Disney World for Spring Break, but Tyler knew he was the only one in his class to go.
Jordan hugs her kitten Chloé as she talks about her trip. Her father “got scared” on the DinoDPutt golf course. “Who knew the dinosaur would spit water?” Bill says. That was the “most funniest” part of the trip, Jordan said.
They went to the Animal Kingdom and Expedition Everest more than once at Disney, all the while staying in a villa. Everything was paid for by the foundation. Bill took “about a thousand” pictures over the week. They got away from some of the harsh realities of Jordan's conditions. Bill was just laid off from a warehouse company, but had an interview Thursday. Emily has insurance at her job. Jordan does qualify for Medicaid, so the medical expenses for all the doctor visits and emergencies and prescriptions are paid for, after they met a $500 deductible and a $1,500 outDofDpocket equipment.She's 9, and she's taking two blood pressure pills. Two pills for her stomach. Two pills for epilepsy, and a pill for attention deficit hyperactivity disorder. She's a little girl on a lot of pills, waiting to grow up big enough to get the surgery to open her arteries up. The MakeDADWish Foundation gave them a week away from it. It's motto says it tries to “enrich the human experience with hope, strength and joy.” After meeting SpongeBob, Micky and Minnie, Goofy and Pluto, Barney, SpiderDMan, etc., Jordan's smile showed her joy.
Jacob Grunewald
At 2 1/2 years of age I noted that Jacob complained of his head hurting. He was treated for sinus infections.
Continue Reading →
Jacob Grunewald
At 2 1/2 years of age I noted that Jacob complained of his head hurting. He was treated for sinus infections. At a 3 year check@up he was noted to be incidentally HTN. He was worked up for kidney involvement and
everything came back negative. Then he had a CT for continued c/o headaches, which showed basilar artery enlargement. MRI findings showed small and large vertebral arteries with enlarged basilar artery enlargement. He had an angiogram which showed 3 high grade stenoses greater than 95%.
Some having the appearance of webbing. His Right internal Maxillary artery is mildly diseased, Right posterior cerebral artery is irregular and Left opthalmic artery is involved. He has white matter changes in the peri@atrial regions with focal areas of leukomalacia. He has 4 right renal arteries and 2 left renal arteries. He previously dissected his LICA and now his LICA is markedly diminished in caliber with focal stenosis or occlucion at the level of the cavernous segment. The intracranial internal carotid artery is reconstituted by collateral flow. Narrowing of the RICA with short segmental stenosis noted on the MRA of the brain in 2004. He has compensatory enlargement of the vetebrobasilar system and presence of pial collaterals. Mild prominence of perivascular spaces in the cerebral white matter most pronounced posteriorly. He was diagnosed in Cincinnati Ohio in July 2000 with FMD He had a Angioplasty of his RICA in June 2001 No strokes since. Questional TIA's since 2001 however.
Aiden Rae Gabel
"All kids have high blood pressure when they are sick", is what my husband was told by the nurse during a 'sick' visit.
Continue Reading →
Aiden Rae Gabel
"All kids have high blood pressure when they are sick", is what my husband was told by the nurse during a 'sick' visit to my then 5 1/2 year old daughter's pediatrician. Aiden had a cold, nasty cough, headache and a slight fever. Her BP was 180/105.
Luckily, my husband caught it and he asked the nurse to take it again, and again, and then had the Pediatrician take it. All four times, it had been around the same, 180/105. We were told to go home and come back in one week. No one seemed concerned about her blood pressure.
I took her back for her follow up and her BP was still around 180/105. I asked the nurse to take it again, it was still high. She brought me to the exam room and looked up her past blood pressures. She said "Well, looks like her blood pressure has always been high so that's normal for her", and turned the computer screen so I could look at it. My first horrifying thought was: "how as parents could my husband and I never have noticed this?". My 2nd thought was: "how could her Doctor not be concerned when her BP had been high for years?".
We were sent home that day having been told she had hypertension and a referral for blood work and an echo at Scottish Rite. We were told no physical activity for her. No PE at school. No running around. No gymnastics or softball (she was playing softball and was on a training team for competitive gymnastics). We were told that would make her headaches go away. Over the course of almost 4 months, including wait time for test results, Aiden had tons of blood work, echos with normal results, renal ultrasounds with abnormal results and an MRI. Aiden had the MRI and the doctor at Scottish Rite told us she had FMD in her renal arteries, primarily the right one and he showed us the 'strand of beads'. "She has what???", my husband and I both said.
He referred us to an AMAZING pediatric nephrologist, Dr. Jernigan, (who, I recently learned, also treats another local child that has FMD) here in Atlanta who we saw right away and immediately put her on Enalipril. While Aiden still had to keep the physical activity to a minimum, she no longer complained about headaches. Dr. Jernigan gave us a little info on FMD but her regular pediatrician had little to no info.
That's when I found the FMDSA website and e[mailed Pam and both were my savior. Pam put me in touch with local Surgeons and we had consults about what to do next. It was decided by Dr. Jernigan and the Surgeons that since the Enalipril was keeping her BP close to normal, and given the size of her arteries, angioplasty was not needed at that time and we were to revisit this when she was 10.
We have had renal ultrasounds every 6 months, and MRI once a year to make sure all is ok. Both of her kidneys are growing fine, and her BP has stayed great on the pills. Last year she was upgraded to seeing Dr. Jernigan once a year and we are to schedule for that appointment in April 2011. We also take her blood pressure at home.
I do not have FMD and as far as I know, no one in my family has it. However, my mother had diabetes and had high BP. She did end up having a kidney transplant due to failure and eventually had a stroke and passed away (before Aiden was diagnosed with FMD). All of those were a result of her diabetes but we wonder if she did have FMD as well.
In reading these stories, I know 100% that we have been very fortunate with Aiden and FMD. Yes, she has been poked and prodded, spent nights in the hospital and couldn't run around for 6 months but there has been nothing major that we have had to worry about thus far. (Knock on wood!) It has now been 5 years and Aiden is a normal 10 year old that takes Enalipril twice a day. She no longer plays softball or gymnastics but is in competition cheerleading and tumbling classes twice a week. You would never know she has any condition. I know that her future will be full of challenges, hospital visits and many tests but I thank God every day for her and that we find a cure for FMD someday!!!!
Shawn and Kristie Gabel-Atlanta, GA
Aiden's Proud Parents
Tracy and Alex Toto
When I was 13, I needed a physical to go to camp over the summer. At that routine physical it was noted that my blood pressure was 180/110.
Continue Reading →Tracy and Alex Toto
While putting on my makeup getting ready to go out to dinner I noticed my right eye was dropping. The
following day I saw my Internist who sent me to my Neurologist. We spent most of the appointment talking about my migraines which seemed to be increasing. He had suggested I have an MRA because of the drooping right eye, but the conversation had gone elsewhere and I was about ready to walk out the door when he said, “Why don’t you have that MRA”. The following morning I had the MRA and nothing could have prepared me for the call from my Neurologist a couple of hours later. I was told they did think I had an aneurysm and needed to have a CTA the following day. My parents had just moved to a Retirement Home in Atlanta, my daughter was scheduled to deliver my second grand son two weeks later and I was starting a
new Interior Design business. Life could not have been better.
The CTA confirmed the aneurysm and I was sent to a Neurosurgeon for further evaluation. That resulted in a Cerebral Angiogram. The recommendation was to do nothing about the Aneurysm. In fact they actually found two, but they were small and highly unlikely to rupture. As so many of us with FMD often say, “I felt like a walking time bomb.” What I didn’t know that day
was that they found much more.
Six months later while reading a book in bed stroke symptoms
began. The right side of my face suddenly went numb, I got up and realized I had a very hard time walking to the bathroom. I tried to google “stroke symptoms” and my right hand was uncoordinated and I had a hard time doing it. Living alone I had not spoken all night so didn’t know until I called my daughter that my speech was very slurred. Once I heard myself talk I made the call to 911. I was very puzzled since I didn’t have any risk factors for stroke. After being diagnosed with a TIA and spending the night in the hospital I decided I needed to get that Angiogram report. I got quite a shock when I saw that I had some disease called Fibromuscular Dysplasia in both Carotid and Vertebral Arteries and also in my Petrous, Cavernous and Supraclinoid
segments of my Internal Carotid Arteries. Then there was more.....
The CT scan they did after the Angiogram showed that I had encephalopathy in my left frontal lobe from previous ischemia.
SCAD FMD
Amy Cavaliere
Young healthy and active when she had a spontaneous coronary artery dissection (SCAD) and went on to also get diagnosed with FMD.
Continue Reading →
Amy Cavaliere
I was a 35-year-old woman, with three kids under 10, a husband who loves me and a very comfortable life. I had never heard of SCAD (Spontaneous Coronary Artery Dissection) and had no idea how it would completely change my life.
That change came on February 1st , 2017 with no warning. I lived a healthy lifestyle – exercise, good diet, and no smoking. My family has no history of heart disease so nothing leading up to this pointed to a potential heart attack.
The morning of the 1st was like any morning except I woke up with pain in my arms and a heaviness in my chest. I became short of breath while I was brushing my 8 year old hair for school. That shortness of breath soon turned into hyperventilating. I assumed it was a panic attack – which I have no history of – and I brushed off the need to have an ambulance called. Good thing my husband disagreed and called 911. I walked onto the ambulance and quickly became unresponsive. My heart had stopped and I was in full blown cardiac arrest. From there the EMT and emergency room nurses and doctors performed CPR and used an AED for 45 minutes. Once my heart was stable I was placed in a medically induced coma and packed in ice bags (hypothermia protocol) and put on a LifeFlight to be flown to Jefferson University Hospital for continued monitoring and care to ensure no neurological damage was done.
There, I stayed on the “Arctic Sun” (hypothermia protocol) for 72 hours to let my brain heal. After eight days of being in a medically induced coma, I battled through a collapsed lung, severe pneumonia in both lungs, blood clots in my leg and heart and finally necrotic tracheal tissue blocking my windpipe which was a result of the traumatic intubation on day one.
After three weeks in the hospital I was discharged with a final diagnosis of SCAD resulting in heart attack and cardiac arrest. I was tested for FMD while in the hospital but it was determined I did not have it.
After recovering at home for many months I decided that for the sake of my children’s future, I needed to find out why this happened to me. My docs were saying we would probably never know. I could accept that answer but only has a last option. I had to dig deeper. So I made an appointment with the world renowned SCAD team at The Mayo Clinic in Rochester, MN. What an eye opening experience!
It was determined at that appointment that I did in fact have FMD, a known link to SCAD, in both my renal arteries and possibly other arteries as well. From Mayo Clinic I was referred to Mt. Sinai in NYC for further evaluation with their FMD team, a leader in Fibromuscular Dysplasia research. This is where things truly came full circle for me because it gave me an answer to WHY this happened. It was confirmed that I have FMD in both renal arteries as well as my left carotid artery which puts me at higher risk for stroke as well. I would have new limitations to adjust to and a new “normal” to accept but it gave me the knowledge of what was happening inside my body. It gave me an answer to why my body betrayed me that day. With answers comes a healing process. These doctors helped to begin this healing process for me that includes learning to trust my own body again.
I never thought that I’d be a SCAD, heart attack, and cardiac arrest survivor at 35 years old. I also never thought that I’d be diagnosed with not one but two incredibly rare diseases all in the same year. This journey hasn’t been an easy one. It still isn’t. But I’m committed to helping others walk this road as so many have helped me and spreading awareness about FMD and SCAD.
Claudia Kime
My name is Claudia, and I am an 8-year survivor of SCAD. I had my 1st SCAD and massive heart.
Continue Reading →Claudia Kime
My actual dissection happened in the hospital two days after my last discharge from the ER.
My husband had been admitted for observation and I was visiting with him. I was immediately
taken to the ER and the Cath lab. The doctor doing the Cath told me my Left Anterior
Descending (LAD) artery dissection 85%. I was stabilized with intra-aortic balloon pump and air
flighted to Johns Hopkins Hospital in Baltimore, MD.
Since the cardiologists and the cardiac surgeons could not come to consensus on how to treat
me, I was medically managed for 3 days. On 3rd day was told that I was stable enough to have
the intra-aortic balloon pump taken out and that I would be going home the next day. I
remember them coming into my room and doing something with the equipment and my chest
pain increasing and then a flurry of activity in my room. A doctor through some forms at me
and told me to sign and that I needed emergency surgery. I started to read them, and he told
me we did not have time for me to read the forms, just sign. I was taken in for emergency
bypass; my family was told I may not survive, and that the next 48 hours were crucial.
After surgery I was in cardiogenic shock; I came out of bypass surgery with temporary
pacemaker and still on the intra-aortic balloon pump. I was out of work for 3 months.
I had my 2nd SCAD and 2nd heart attack in September 2012 two weeks after returning to work
from my first heart attack and while driving home. I did not know at the time that it was
another SCAD – the diagnosis was missed by Johns Hopkins Hospital. It was found in 2017 at
Mayo Clinic that the 2nd heart attack was caused by a dissection in my Right Coronary Artery
(RCA).
In 2015 I started suffering with chest pain. My cardiologist took me to the Cath lab and noticed
a narrowing in my LAD right below where the bypass tied in. We tried medications to alleviate
my pain, but I ended up with a stent in my LAD. The cardiologists believe the blockage was
caused by my bypass sutures (my native artery healed and started working again and the
sutures were causing blockage).
I was diagnosed with Fibromuscular Dysplasia (FMD) in multiple arteries 2015 by Dr. Jeffrey
Olin. I am monitored yearly for my FMD.
Dawn Marisch
I was diagnosed with FMD in October of 2011, following a ruptured splenic aneurysm that nearly took my life the prior June.
Continue Reading →
Dawn Marisch
I was diagnosed with FMD in October of 2011, following a ruptured splenic aneurysm that nearly took my life the prior June. It raised so many questions for myself and my family as I slowly recovered after several weeks in the hospital. We learned that my renal, hepatic, and vertebral arteries were impacted. In the months to follow I slowly rebuilt my strength. With an effort to learn more and find support for patients, we found the FMDSA. The connection, support, and information resources, provided hope. Life slowly returned to 'normal'. We monitored the impacted areas annually and were pleased with limited change, until September of 2018.
I woke one morning with unexplained lower back and abdominal pain. Although the pain was dull, it was constant and prevented me from my daily activities. Ultimately, my doctor recommended a trip to the emergency room, and so I went. Because of my history, chest and abdominal scans were ordered. The doctor entered my room and told me the scans indicated a dissected aorta, requiring immediate surgery. As the team prepped for surgery my interventional specialist was contacted. Upon his review, the surgery was cancelled, I was admitted to the hospital and treated medically. I have continued the medicinal regimen, with close monitoring, and have remained stable. I cannot stress enough the importance of establishing a regular care team that knows you well and can respond in times of serious medical events. Life again returned to 'normal'.
Sadly, on March 7, 2020, my oldest daughter of three experienced a sudden rupture of an undiagnosed aortic dissection and passed away. Our family is devastated by the loss of our beautiful Allyson Jane. Her mantra was "Throw all the good you can out into the world, and see what comes back". Although our lives will never return to 'normal', Ally was and always will be a ray of sunshine in our lives that drives us forward to raise awareness, support research, and seek answers for the rare disease community.
Jeannine Seery
My journey to FMD has been a long one, with many winding roads and dead ends.
Continue Reading →
Jeannine Seery
Sixteen years ago, I had a massive heart attack at age 34. I was two weeks postpartum, with no history of heart disease and no risk factors. In the blink of an eye, I went from being a healthy young mother to a critically ill patient awaiting emergency bypass surgery to repair a coronary artery that had blown out. My world crashed down around me as I wondered if I would live long enough for my infant daughter to remember me.
I recovered from that surgery and woke up with endless questions and very few answers. My doctors suspected that I had experienced something called a SCAD, which led to my sudden heart attack.
My recovery was slow and frightening as I adjusted to a life with newfound uncertainty. How and why did this happen to me? Pregnancy and childbirth was supposed to be a ‘normal’ event- mine resulted in a massive heart attack that compromised my life. What made me different?
I began a long journey looking for answers. I visited rheumatologists, hematologists, endocrinologists. They found nothing. Nobody could tell me why I had a SCAD. I lived in constant fear that my body would turn on me again and perhaps this time I wouldn’t live to tell about it.
Last year, fifteen years after my SCAD event, I sought help from a neurologist for my persistent chronic migraine headaches. Listening to my story, she asked if I’d ever seen a Genetic Cardiologist. I had no idea that there was such a thing. She suspected that there might be a link between my migraine headaches and my SCAD. Needless to say, I was intrigued.
A series of events brought me to the office of Dr. Daniella Kadian-Dodov where I was diagnosed with FMD- over sixteen years after my SCAD. I have evidence of FMD in my carotid, femoral and renal arteries and Dr. Kadian-Dodov suspects that FMD was what led to my postpartum SCAD almost two decades ago.
This diagnosis has brought me peace. I finally have an explanation for my SCAD and I have tools to manage the illness that caused it. I have found support and knowledge in the brief time since my diagnosis in online support groups for FMD and through the FMD Society. I only regret that it took such a long time for my diagnosis. Had my doctors known about FMD, I could have avoided many sleepless nights worrying about the random event that almost took my life, one that turned out not to be a random event at all.
PLEASE NOTE: FMDSA is not responsible for the accuracy of our patient stories, nor any medical conclusions contained therein. The purpose of this section is simply to provide a forum for our members to tell their stories in their own words.
FMD Clinics
If you would like to be evaluated at one of the FMD clinics below, please contact them directly. Please note that not all **clinics participate in the US Registry for FMD, for a list of registry centers currently participating
visit the US Registry Page on our website.

Baptist Cardiac and Vascular Institute
The FMD program at the Baptist Cardiac and Vascular Institute in Miami provides patients with FMD specialized care by a multidisciplinary team of clinicians’ experts in the evaluation and management of patients with FMD. For more information, visit https://cardiovascular.baptisthealth.net/miami-cardiac-and-vascular-institute/research-and-innovation.
To schedule an appointment with Dr. Barry Katzen or Dr. Ian del Conde, please email RaulH@baptisthealth.net or MariaGo2@baptisthealth.net, or call 786-267-5467 / 786-843-2309.
Cleveland Clinic
The Cleveland Clinic FDM Clinic is a multi-disciplinary clinic based out of their Vascular Center.
Please call 216-445-3689 or 800-223-2273 to schedule an appointment.
Emory Healthcare - Fibromuscular Dysplasia Program
We are excited to share that Dr. Bryan Wells of Emory Hospital in Atlanta has announced their new Fibromuscular Dysplasia Program. The Emory FMD Program has a multispecialty team that provides comprehensive, coordinated care in all aspects, including evaluation, diagnosis, genetics, medical treatment, invasive procedures (when needed), and disease surveillance.
To schedule an appointment please call 404-686-8203. For more information on the FMD Program at
Emory please visit their website

Johns Hopkins Hospital
The Johns Hopkins Fibromuscular Dysplasia Clinic is a multidisciplinary clinic dedicated to the diagnosis and treatment of FMD. Overseen by Vascular Medicine and Nephrology, the clinic offers expert management from Vascular Medicine, Nephrology, Neurology, Cardiology, Vascular Surgery, and Interventional Radiology. For an appointment, please contact Dr. Elizabeth Ratchford, MD (evr@jhmi.edu; 443-997-0270) and or Dr. C. John Sperati, MD, MHS (jsperati@jhmi.edu; 410-955-5268) for more information, please visit their website.

Massachusetts General Hospital Vascular Center
The Fibromuscular Dysplasia Program at the Massachusetts General Hospital Vascular Center provides patients with specialized care for Fibromuscular Dysplasia (FMD). Massachusetts General Hospital is one of the only hospitals in the United States to bring together a multidisciplinary team of clinicians dedicated to diagnosing, treating and helping patients manage FMD. For more information, visit www.massgeneral.org/FMD or call 877-644-8346.

Mount Sinai Heart Center for Fibromuscular Dysplasia Care and Research
The prevalence, cause, prognosis and optimal treatment of fibromuscular dysplasia (FMD) is not known. Despite an improved clinical understanding of the disease, through initiatives such as the United States Registry for FMD, there has been little progress in understanding the biologic cause of FMD since its first description in 1938. Data from the registry suggests that many patients had subtle manifestations of FMD for years before diagnosis and treatment.
There are a number of similar features that occur in family members of patients with FMD. This suggests that genetics play a significant role in the cause and/or predisposition for developing FMD.
To begin to identify the cause and eventual treatment of FMD, we have formed “The Mount Sinai Heart Center for Fibromuscular Disease Care and Research” with the goal of sorting out the cause and full clinical spectrum of FMD. We have a multidisciplinary team of experienced clinicians dedicated to treating patients with fibromuscular dysplasia. For an appointment email annette.king@mountsinai.org or jeffrey.olin@mountsinai.org or call 212-241-9454 for an appointment with Dr. Jeffrey Olin or Dr. Daniella Kadian-Dodov.
University Hospitals Harrington Heart & Vascular Institute, Cleveland, Ohio
Our Fibromuscular Dysplasia and Arterial Dissection Program is led by one of the world’s most renowned authorities on these increasingly common vascular conditions, Heather Gornik, MD. This interdisciplinary team includes specialists in vascular medicine, endovascular therapies, vascular surgery and advanced imaging. Our program is recognized as a site for both the North American Registry for FMD and iSCAD Registry. Dr. Gornik, along with national and international colleagues from the Society for Vascular Medicine and the European Society of Hypertension, co-authored the first international consensus document on the diagnosis and management of FMD, co-published in the Journal of Hypertension and Vascular Medicine. Recognizing the need for patient and family support, our program hosts online quarterly group sessions, providing a forum for education and open discussion.
For more information, visit: https://www.uhhospitals.org/services/heart-and-vascular-services/conditions-and-treatments/vascular-disease/fibromuscular-dysplasia-program
To schedule an appointment with Dr. Heather Gornik, visit: https://www.uhhospitals.org/doctors/Gornik-Heather-1316030802

University of Illinois Medical Center
The University of Illinois FMD Clinic is a multi-disciplinary clinic based out of their Stroke Center.
For appointments, contact Jenna Reeh at 312-355-9846.

The University of Kansas
The hospital’s Fibromuscular Dysplasia program provides patients with specialized care for FMD. Our multidisciplinary team of specialists, led by Kamal Gupta, MD, offers advanced diagnosis, treatment and long-term management of FMD.
For more information, call 913-945-1227 or visit kumed.com/cardiology.

University of Michigan
The University of Michigan Health System faculty and staff have had a longstanding interest in the management of fibromuscular dysplasia (FMD) and now offer a combined, multidisciplinary clinic for patients diagnosed or suspected of having fibromuscular dysplasia (FMD). If you would like to be seen at the University of Michigan, call the Cardiovascular Call Center at 1-888-287-1082 and ask to be seen by one of the physicians who specialize in managing patients with FMD.
University of Virginia
The University of Virginia Fibromuscular Dysplasia program is a multi-disciplinary clinic coordinated by Vascular Medicine physician Dr. Randy Ramcharitar who in conjunction with vascular interventional radiologists, vascular neurologists, vascular surgeons and other specialties provide state of the art diagnostic and therapeutic options to treat people with FMD. The program is very active with the registry and other research related to FMD.
Please call 434-243-1000 to schedule an appointment.
Seattle Children’s Hospital
Seattle Children’s Hospital serves the largest region of any children’s hospital in the country.
Contact Dr. Susan Halbach, Pediatric Nephrologist, at 206-987-2542

Prisma Health Upstate
Dr Andrew Bryant Dicks has special interests include peripheral intervention for aortic aneurysm, carotid, renal, and lower extremity disease. Special expertise in fibromuscular dysplasia and congenital vascular diseases are unique to the region. Greenville, SC 864-454-8272

North Central Heart
Sioux Falls, SD, Dr. J. Michael Bacharach is a cardiologist, vascular medicine and intervention specialist. 605-977-5000
University of Colorado
Dr. Kevin Rogers specializes in vascular disease, stroke, hypertension, and performs endovascular treatment. 720-848-5300

Stanford Vascular Clinics
Stanford, CA, Dr Eri Fukaya is a vascular medicine specialist and surgeon. 650-725-5227

Dr. Kambiz Zorriasateyn, MS FACP RPVI
Vascular Medicine
FMD/SCAD Clinic
Northshore Cardiovascular Institue
Location: 1000 Central Street Suit 730 Evanston, IL 60201
Appointment: 847-663-8050 – Mrs. Tamar Sutherland
Fax: 224-251-4407
Dr. Kambiz Zorriasateyn of NorthShore University Health System is a specialist in the areas of FMD and SCAD and would love to see you!
Support Groups
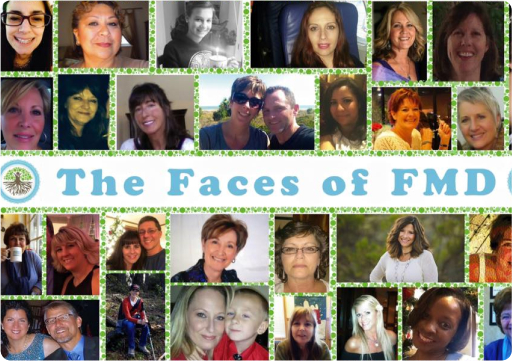
FMDSA Online FMD/SCAD Inspire Support Group
Please join us on our FMD Inspire support group. To be taken to our group, click here. Post your own questions or just read those from others on a range of FMD topics.

Regional FMDSA Networks
FMDSA is in the process of organizing Regional Network Volunteers/ Groups across the country. If you do not see your City or State listed, please check back soon as we are in the process of adding more groups. Please note these groups are informal and run by volunteers, many who also have FMD.
The volunteers/groups have been formed to offer support for affected persons and their families and to foster local efforts to further the FMDSA mission. It gives you the opportunity to meet others who have also been diagnosed with fibromuscular dysplasia and or spontaneuous coronary artery dissection (SCAD) the opportunity to promote public and professional awareness of the disease in your community. For questions about the groups please contact our Admin at admin@fmdsa.org

The Tree as Our Symbol
The tree has always been a universal symbol of many things, including wisdom, protection, and strength. Specifically, in terms of Fibromuscular Dysplasia, the tree’s branches signify the arteries affected by this disease, and life itself.
Follow our Facebook
Regional Network Volunteers/ Groups
Alabama
Mary Jo Hicks at hicksjo@bellsouth.net
Arizona
Carol McGatha at cmcgatha@cox.net
Nina Verstraete at nina.verstraete.fmdsa@gmail.com
California (Northern)
Robin Berlin at rberlinrd@gmail.com
Colorado
Cami Bremer at cami.bremer@gmail.com
International Volunteer Network and Groups
Belgium
Cathlin Jamison at cathlin.fmd@gmail.com.
FMD-Be website, click here
Brazil
Robsom Alvarenga at robsom@gmail.com
Canada
Rochelle DesRochers at rochelle.desrochers@fmdsa.org
Hungary
Eszter Pechy Alvarenga eszter.pechy@gmail.com
Ireland
You can find the UK and Ireland group on Facebook.
Israel
Lena Reznik @ lenar1982@gmail.com
Netherlands
Madelon Bouwmeester, website click here
New Zealand
Cherrill Bell at cherrypie@nowmail.co.nz
Poland
Kuksa Duksa at babikland@interia.pl
South Africa
Ashleigh Botha at ashy.botha@gmail.com
Switzerland
Nina Verstraete nina.verstraete.fmdsa@gmail.com
UK




 Since ancient times and across many cultures, the tree has long been a symbol of many things, including wisdom, protection, strength, inter-connectivity, and life itself. We’ve chosen the tree to represent the Fibromuscular Dysplasia Society of America for these reasons, and because the tree’s branches and roots signify the arteries affected by this disease. The tree’s branches, reaching upward and outward, provide protection and shelter, and represent our mission to help those who’ve been diagnosed with FMD. Trees, strengthened by their continuously spreading roots, symbolize how as we grow together we are stronger and more resilient. As with its growth from a delicate sapling to a giant robust tree, and as its branches and roots grow and spread, the tree symbol represents how we’ve evolved and continue to promote research, education and patient support throughout the years. Together we can achieve much, as we strive to reach for the sky.
Since ancient times and across many cultures, the tree has long been a symbol of many things, including wisdom, protection, strength, inter-connectivity, and life itself. We’ve chosen the tree to represent the Fibromuscular Dysplasia Society of America for these reasons, and because the tree’s branches and roots signify the arteries affected by this disease. The tree’s branches, reaching upward and outward, provide protection and shelter, and represent our mission to help those who’ve been diagnosed with FMD. Trees, strengthened by their continuously spreading roots, symbolize how as we grow together we are stronger and more resilient. As with its growth from a delicate sapling to a giant robust tree, and as its branches and roots grow and spread, the tree symbol represents how we’ve evolved and continue to promote research, education and patient support throughout the years. Together we can achieve much, as we strive to reach for the sky.